Degenerative Scoliosis with Osteoporosis and Spinal Stenosis: Surgical Planning and Survey of the Supporting Literature.
Patrick K. Cronin, MD and Jay M. Zampini, MD
The authors report no conflict of interest related to this work.
©2019 by The Orthopaedic Journal at Harvard Medical School
We report the case of a 73-year-old female with degenerative scoliosis with positive sagittal balance, osteoporosis, and functional impairment secondary to lumbar spinal stenosis. Principal considerations in selecting surgical management include comorbidities, fitness for surgery, bone mineral density, sagittal plane alignment, and concordance of history, physical examination, and imaging findings.
LEVEL OF EVIDENCE Level V Case Report
KEYWORDSDegenerative scoliosis, positive sagittal balance, lumbar spinal stenosis, osteoporosis
Degenerative scoliosis (DS) commonly manifests in two populations: those with a complex spinal deformity whose primary symptoms arise from coronal and sagittal imbalance and a second population of patients with symptoms usually arising from lumbar spinal stenosis (LSS) who also have a degenerative coronal plane deformity. For this second group, the management of LSS is complicated by the coincidence of scoliotic deformity.1 Literature emphasizing the superiority of surgical outcomes for treatment of LSS indicate that, in this latter cohort, neurologic decompression should remain a primary treatment consideration.2-5
In general, the surgical options for DS with LSS involve decompression alone, decompression with short segment fusion, or deformity correction with long-segment fusion, potentially including interbody fusion. Traditionally, decompression alone has been avoided due to concern for worsening the deformity.6,7 Decompression accompanied by non-instrumented8 or instrumented fusion9,10 has been reported with focus on the importance of sagittal balance.11,12
Perioperative risk for surgical treatment of DS can be significant, and careful patient selection with maximal medical optimization is important to minimize complications.13-15 Major complications such as instrumentation failure, deep infection, vascular injury, and neurologic deficits may occur in as many as 10% of adult deformity surgeries and can negatively impact patient function for up to a year after the index surgery.15 The ability to achieve a successful outcome following surgery is also limited by patient comorbidities and bone mineral density.16,17 While many surgical risk factors and complications have been described,14,15 high quality evidence to guide surgical planning is lacking. We report a case here of spinal stenosis with concomitant degenerative scoliosis that is illustrative of the complexity in surgical decision-making and convene a panel of nine spine surgeons with independent practice experience ranging from six months to twenty-five years to discuss their interpretation of the literature and treatment approach.
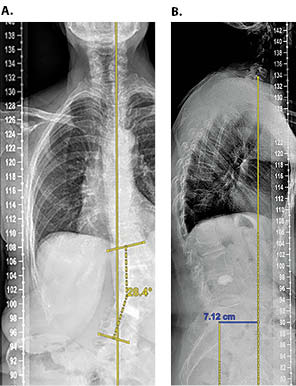
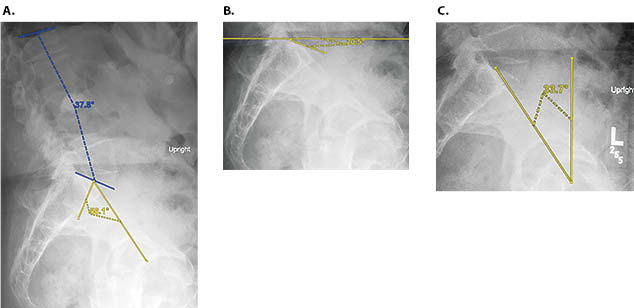
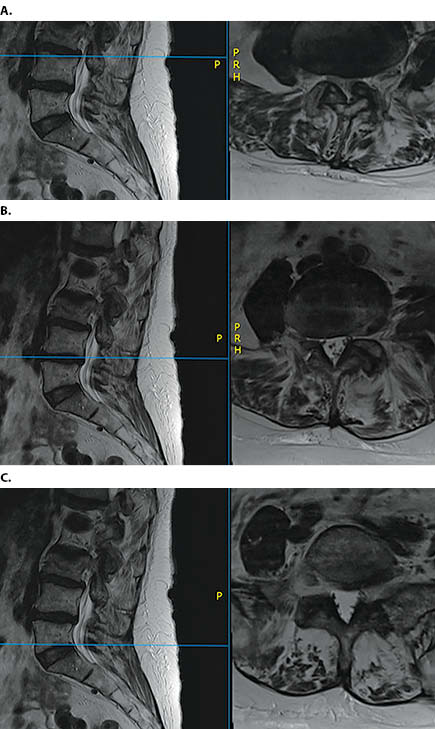
Written informed consent was obtained from the patient to discuss and publish de-identified information. A 71-year-old female presented with nearly 6 months of acute on chronic worsening of low back pain with pain radiating down her left anterior thigh. She also reported worsening ambulatory endurance with symptoms consistent with neurogenic claudication. On a self-reported scale, her back pain was 7/10, and her leg symptoms were 8/10. Her symptoms were refractory to physical therapy, activity modification, and oral pain medications. She had a short period (<2 weeks) of relief following an epidural steroid injection. Past medical history is notable for L3 vertebral insufficiency fracture treated with kyphoplasty, stage III chronic kidney disease, hypertension, and major depressive disorder. The patient had completed a one-year course of teriparatide for treatment of osteoporosis with pre- and post-treatment dual X-ray absorptiometry (DEXA) scans revealed a T-score of -2.7, consistent with osteoporosis. Physical examination was remarkable for positive sagittal balance on standing exam, symmetric shoulder height and leg length, and slight paraspinal prominence on Adam’s forward bend test. She was neurologically intact with respect to sensation and motor function and had a negative straight leg raise test bilaterally. Standing 32 inch radiographs are shown in Figure 1 and demonstrate coronal deformity of approximately 28° and a positive sagittal vertical axis (SVA) of approximately 7 cm. Other radiographic measurements are shown in Figure 2 including: a) lumbar lordosis (38°) and pelvic incidence (56°), b) sacral slope (21°), and c) pelvic tilt (34°). Magnetic resonance images are shown in Figure 3 and demonstrate multilevel degenerative changes with central and lateral recess stenosis most severe at L3-L4 on the left side.
The patient’s condition is complex and includes the following treatment considerations: pain and functional impairment secondary to lumbar spinal stenosis; a structural deformity of the spine with degenerative scoliosis and positive sagittal balance; and severe osteoporosis.
The panel members unanimously agree that surgical intervention is indicated for treatment of the patient’s pain and functional impairment given that she has been unable to achieve significant and sustained improvements with nonsurgical treatment.
Planning the specific surgery in this case, however, presents several challenges. Her clinical presentation suggests that lumbar spinal stenosis with neurogenic claudication produces the most significant impact on her overall function. Direct spinal decompression is therefore the primary goal of surgery.
The surgical plan must also take into account the patient’s deformity resulting from both degenerative scoliosis and sagittal imbalance. SVA is critical for optimizing clinical outcomes, and a high SVA can lead to loss of function.11,17 Even in asymptomatic individuals, ageing involves the development of some forward sagittal alignment with an increasing SVA. Profiling of the asymptomatic, ageing population also demonstrates a decrease in lumbar lordosis (LL) according to the formula:19
- LL = 32.9 + 0.6(pelvic incidence) – 0.23(age)
One could interpret this observed change in lumbar lordosis as compensatory for increasing SVA to maintain upright posture and forward horizontal gaze. Assuming the external validity and generalizability of this formula to the larger population, our patient lacks approximately 12° of lumbar lordosis compared to age matched asymptomatic individuals.
The flexed lumbar posture assumed by patients with lumbar spinal stenosis (i.e. positive sagittal balance) is hypothesized to occur as a protective mechanism to avoid neurologic symptoms. In patients with LSS without degenerative scoliosis, decompression alone has been shown to improve sagittal imbalance in up to 70% of patients.20 These findings were replicated in patients with modest degenerative scoliosis (Cobb angle <20 degrees) and concomitant scoliosis with decompression alone leading to improvement in post-operative sagittal spinal alignment.21 Whether these results can be generalized to patients with curves greater than 20 degrees, such as our patient (Figure 1), is not clear. While more invasive techniques of sagittal imbalance correction are frequently utilized—including interbody fusion devices, osteotomies and posterior instrumented fusions—these other methods are not ideal for individuals with poor bone quality.22-24
In terms of decompression alone, options include traditional open decompression and minimally invasive procedures. Microendoscopic laminotomy and foraminotomy have been proposed as minimally invasive approaches for patients with lumbar spinal stenosis with neurogenic claudication and associated degenerative scoliosis.21,25 In a Japanese study enrolling 438 patients, 122 patients were followed for a mean 2.4 years after microendoscopic decompressive surgery with observed Japanese Orthopaedic Association (JOA) recovery rate of 47.6%; smaller improvements in functional outcome were observed in patients who had more severe deformity or experienced progression of the Cobb angle.21,25
Comparison of decompression with limited instrumented fusion (1-2 levels), decompression with fusion of the entire curve, and decompression alone in 85 patients with an average Cobb angle of 25° demonstrated similar, but slightly improved SF-36, Oswestry Disability Index (ODI), and Roland Morris Scores in the limited fusion group, despite no change in the Cobb angle.26 The importance of this observed 7.6 point ODI decrease and 1 point SF-36 increase with limited fusion is suspect given that an ODI score decrease of 12.8 and improvement in SF-36 of 4.8 has shown to be the threshold of clinical relevance following lumbar surgery.26,27 Patients who underwent decompression alone had the lowest complication rates: 10% for decompression alone, 40% decompression with limited fusion, and 56% in the full fusion groups.26
Several predictors of curve progression include intervertebral disk degeneration, lateral vertebral translation (≥ 6mm) and deformity greater than 20 degrees.21,28 Given that several of these factors can be observed in our patient (Figure 1), a limited fusion procedure, rather than decompression alone, can be supported as a reasonable choice.
The objective measurements in this case suggest that it is ambiguous whether decompression alone will improve the patient’s sagittal or coronal profile and may lead to worsening deformity without stabilization. This patient, the panel agrees, will therefore benefit from spinal fusion in addition to decompression. The presence of osteoporosis must also be taken into consideration when planning for a fusion procedure, especially in the setting of instrumentation. The diagnosis of osteoporosis has been made via DEXA scan in our patient, and quantitative CT evaluation of the lumbar spine could be used to make a more accurate determination of bone mineral density.29-31 Given that our patient has already sustained a vertebral compression fracture, she meets diagnostic criteria for severe osteoporosis.32,33
Once osteoporosis is established by fragility fracture, FRAX, or T-score, early evidence suggests that teriparatide may be of some clinical utility. A 12 month course of once daily 20 μg teriparatide has been shown to increase lumbar spine bone mineral density (BMD) by 11%.34 In a prospective cohort of 1,996 Japanese patients undergoing treatment at the aforementioned dose for 24 months, a 56.4% reduction in the odds ratio for fracture was seen at 6-12 months, 51.6% reduction at 12-18 months, and 58.8% reduction at 18-24 months without any notable adverse effects.35 It has not been shown in humans whether teriparatide increases lumbar spine fusion rates following surgery. Administration in rodent models does appear to improve post-operative fusion rates with some studies showing over a four-fold increase in fusion rates;36,37 these results appear to be retained in rodents with pre-operative osteoporosis.38
Because of her medical comorbidities and osteoporosis, this patient has a complication rate nearing 70% in some studies if she were to undergo an instrumented decompression and fusion.39 The risk of hardware failure in long fusion constructs has been posited to be due to increased load and motion at the last instrumented vertebrae.40 Some surgeons have advocated cement augmentation of the upper one or two instrumented vertebrae.41 A double-trajectory method for pedicle screw insertion has been employed by some to increase fixation in osteoporotic bone.42 Extending the caudal fixation to the sacrum has been shown to improve sagittal correction but at the expense of being a longer, more invasive procedure with a higher major complication risk.43 Non-instrumented fusion has the benefit of reducing operative time and the risks associated with instrumentation, including proximal junctional kyphosis. These benefits are at the cost of possible blunting of the postoperative improvement secondary to residual spinal deformity; consistent with results after decompression without fusion for DS with stenosis.44
The panel concludes that a decompression and limited fusion without instrumentation may be the best overall option for this patient.
The authors would like to acknowledge Christopher M. Bono, MD,1 Thomas P. Cha, MD,1 Stuart H. Hershman,MD,1 James D. Kang, MD,2 Melvin C. Makhni, MD,2 Andrew K. Simpson, MD,2 Andrew P. White, MD,3 and Umesh S. Metkar, MD3.
1Massachusetts General Hospital, Department of Orthopaedic Surgery, Boston, MA
2Brigham and Women’s Hospital, Department of Orthopaedic Surgery, Boston, MA
3Beth Israel Lahey Health, Department of Orthopaedic Surgery, Boston, MA