Volar Dislocation of the Fifth Carpometacarpal Joint Mistaken for Radial Collateral Ligament Injury
Ryan C. Xiao, MD, Derek S. Stenquist, MD, George S.M. Dyer, MD, FACS
The authors report no conflict of interest related to this work.
©2019 by The Orthopaedic Journal at Harvard Medical School
Isolated dislocation of the fifth carpometacarpal (CMC) joint is an uncommon injury that can be missed. The purpose of this paper is to present a case of delayed diagnosis of volar dislocation of the fifth CMC joint and to review the existing literature. The injury was initially mistaken for a radial collateral ligament tear on clinical exam due to malrotation of the digit and a history that pointed to an injury at the level of the metacarpophalangeal (MCP) joint. Definitive management included open reduction and internal fixation with a tension band suture and K-wire construct. A high level of suspicion and careful interpretation of imaging are essential to ensure accurate diagnosis and management of these injuries.
LEVEL OF EVIDENCE Level V Case Report
KEYWORDSCarpometacarpal, CMC, dislocation, fifth, volar
Isolated dislocation of the fifth carpometacarpal (CMC) joint is uncommon and can be easily missed.1 On clinical exam, volar dislocations may be missed more often than dorsal dislocations because the dislocation can be masked by palmar swelling and the soft tissue of the hypothenar eminence. The purpose of this paper is to present a case of delayed diagnosis of isolated volar dislocation of the fifth CMC joint managed with open reduction and internal fixation with a tension band suture and K wire construct and to review the literature for this uncommon diagnosis.
A 62-year-old right-hand dominant man presented ten days after falling during a tennis match and jamming the throat of his tennis racket into the web space between his right ring and small fingers. Initial clinical examination demonstrated resting abduction of the fifth digit. The original interpretation of his right hand radiographs from an outside hospital did not demonstrate evidence of fracture or dislocation. He underwent closed treatment with buddy taping of the long, ring, and small fingers for presumed radial collateral ligament tear of the small finger metacarpophalangeal (MCP) joint. MRI of the right hand was reported to demonstrate this suspected radial collateral ligamentous injury.
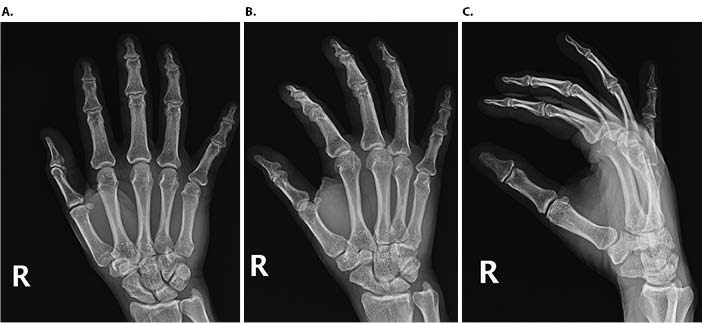
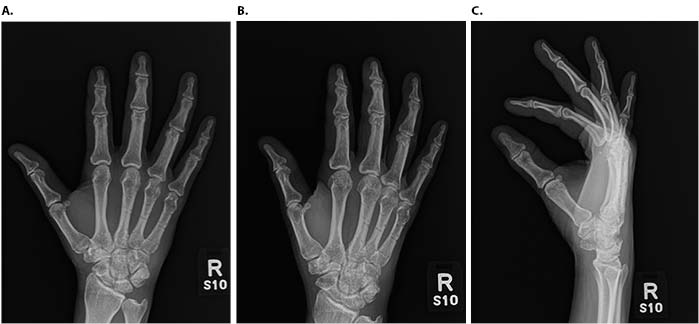
The patient presented to the orthopaedic clinic several days later with difficulty flexing the small finger and malrotation of the digit. Examination of the right hand revealed swelling and resolving ecchymosis over the ulnar aspect of the palm, resting abduction and pronation deformity of the fifth digit (Figure 1), tenderness over the fifth MCP and CMC joints, and instability at the fifth CMC joint. There was no evidence of sensory, motor, or vascular deficit.

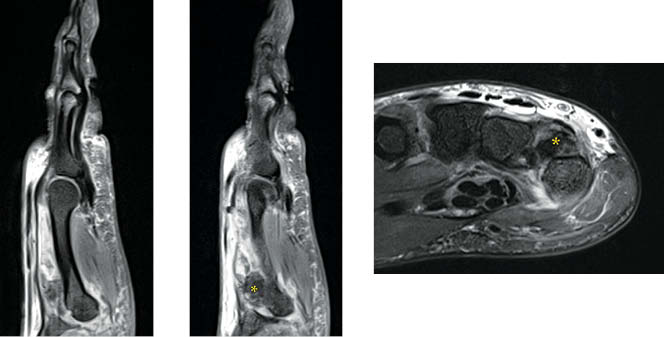
Review of the original anteroposterior (AP), oblique, and lateral injury radiographs of the right hand revealed subtle dislocation of the small finger CMC joint seen on the AP view (Figure 2). Right hand MRI revealed a high-grade partial tear of the small finger MCP radial collateral ligament and an ulnopalmar dislocation of the fifth CMC joint that was missed on the initial interpretation (Figure 3).
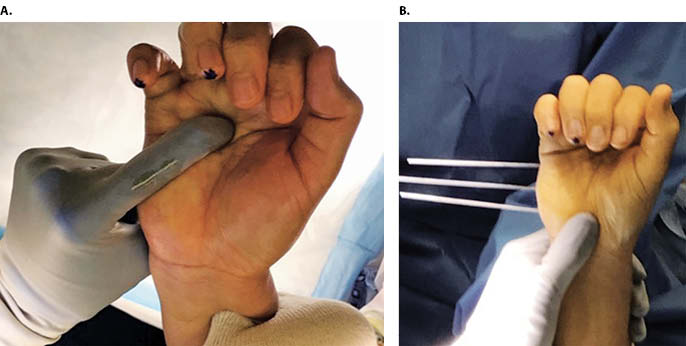
Closed reduction in the office under local block was unsuccessful. The patient was brought to the operating room for open reduction with percutaneous pinning under regional block. Dorsal exposure over the base of the small and ring finger metacarpals allowed visualization of the joints. An avulsed rim of bone and the associated capsular tissue was interposed dorsally causing a block to reduction. Retrieval of these structures allowed reduction of the fifth CMC joint under direct visualization (Figure 4). After anatomic reduction, a tension band suture was placed dorsally across the fifth CMC joint for direct fixation, incorporating the avulsed capsule. This construct was then protected with four 1.6 mm K wires placed from the ulnar side of the hand across the ring and small finger metacarpals into the long finger metacarpal with good restoration of the clinical cascade (Figure 5 and Figure 6). The hand was immobilized in an ulnar gutter splint in the intrinsic plus position. At the two week post-operative follow-up, the patient was transitioned into a cast for four weeks of additional immobilization. At the six week follow-up, there was no evidence of recurrent dislocation or subluxation, and the K wires were removed. The patient then began occupational therapy for range of motion. By the 12 week follow-up, he demonstrated clinically normal hand function and had returned to playing tennis with no residual pain or functional deficits (Figure 7).


CMC joint dislocations account for <1% of hand injuries and often present with associated fractures or injuries to additional digits as a result of significant force.2,3 Isolated CMC joint dislocations are unusual and can occur in either the dorsal or volar direction. There are 16 reports of isolated volar dislocations of the fifth CMC joint in the English language literature with the earliest case described in 1918 by McWhorter.1,4,13-18,5-12
As initially described by Nalebuff, volar dislocations of the fifth CMC can be further subdivided into radiopalmar and ulnopalmar dislocations, each with different associated ligamentous and tendinous injuries.8 The fifth CMC joint between the hamate and fifth metacarpal is stabilized by the pisometacarpal, dorsal carpometacarpal, volar carpometacarpal, and intermetacarpal ligaments. The intermetacarpal ligament is believed to be the primary restraint.15 Tendons of the extensor carpi ulnaris and flexor carpi ulnaris also attach to the base of the fifth metacarpal. In radiopalmar small finger CMC dislocations, the injury disrupts all tendinous and ligamentous support, making these injuries particularly unstable. Ulnopalmar dislocations typically maintain the integrity of the pisometacarpal ligament and tendinous support, which may prevent excessive displacement and make accurate diagnosis difficult.15
CMC dislocations often have a delayed presentation and require a high degree of clinical suspicion for accurate diagnosis.1 Volar CMC dislocations of the small finger can be especially difficult to diagnose clinically as the dislocation can be masked by palmar swelling and the soft tissue of the hypothenar eminence.16 Lateral radiographs of the hand are necessary to evaluate the fifth CMC joint, but subtle dislocations can be easily missed on routine radiographs. Nakayama et al. suggest that an oblique view (with the hand at 30° of supination) may show the relationship between the fifth metacarpal base and the adjacent bones.16 Yamakado et al. described the use of stress x-rays (with traction and axial compression) to make the diagnosis.15 As in this case, the exam and even advanced imaging may be misinterpreted as collateral ligament injury due to the resulting angular deformity or malrotation of the digit. The overlap of carpal bones on lateral x-ray makes imaging difficult to interpret. Computed tomography (CT) evaluates articular relationships better than x-ray or MRI and can be useful for pre-operative planning.19,20 A CT scan can also be obtained to rule out CMC dislocation if there is malrotation of a digit on clinical exam and suspicion for CMC dislocation in the emergency department.
Hodgson and Shewring proposed using metacarpal cascade lines on posteroanterior (PA) radiographs of the hand to better identify CMC dislocation injuries..21 Comparing 25 uninjured hands to 25 examples of fourth and fifth CMC dislocations, they described a pattern such that lines through the longitudinal axes of the second through fifth metacarpals on the PA view will intersect at a common point proximal to the radial styloid process in uninjured hands. In the hands with CMC dislocations, the four metacarpal axis lines did not intersect at a common point, with disruption of the pattern by the affected metacarpal. When study participants were taught to evaluate metacarpal cascade lines and were presented the same 50 images, the authors found 92% sensitivity and 96% specificity for identifying CMC dislocations. When evaluating the pre-operative AP radiographs in this case using the metacarpal cascade lines, there is divergence from the normal cascade pattern in Figure 8, suggesting a CMC dislocation at the small finger.

Dislocations of the fifth CMC joint have been treated successfully with closed reduction and casting in the acute setting up to two days after initial injury.12,14,18,22 Closed reduction is performed with pressure directly over the base of the dislocated CMC joint while simultaneously applying longitudinal traction to the affected fingers. In 1985, Berg described a case of fifth CMC joint dislocation successfully managed with closed reduction and casting. Though he noted re-dislocation as soon as traction was released, the reduction was able to be maintained in an ulnar gutter splint in the intrinsic plus position.12 In 2011, Storken et al. described four additional successful cases of closed reduction of fourth and fifth CMC joint dislocations, all treated within eight hours of injury.22 Closed reduction can prove difficult in cases of delayed presentation. Zhang et al. noted inability to reduce fracture-dislocations of the fourth and fifth CMC joints presenting over two weeks post-injury due to the formation of scar tissue.23 In an open reduction of a fifth CMC joint dislocation seen four weeks after initial injury, Buzby similarly noted interposed scar tissue necessitating open reduction and debridement.5 This was the case with this patient, who presented ten days after injury with interposed capsular tissue and bone fragments.
Surgical treatment is often required due to the unstable nature of these injuries, and various techniques have been described. Even after successful reduction, maintaining the reduction may prove challenging when traction is released.8,12,16 Percutaneous pinning using K wires after closed versus open reduction can prevent re-dislocation due to loss of integrity of the carpometacarpal and intermetacarpal ligaments with ulnopalmar dislocation.4,8,11,15-17 In 1918, McWhorter achieved reduction via a dorsal incision, sutured the base of the fifth metacarpal to the hamate, and placed the patient in a splint.3 Nalebuff treated an isolated volar dislocation of the fifth CMC joint with open reduction and two K wires inserted horizontally from the base of the fifth metacarpal into the shaft of the fourth metacarpal.8 Tountas described percutaneous fixation with two K wires inserted along the metacarpal shaft into the hamate.11 Nakayama et al. treated two cases in the same manner, adding a K wire from the fifth metacarpal to the fourth for stability in one case.16 In persistently symptomatic cases, fusion of the fifth metacarpal to the hamate or interposition arthroplasty have been described.11 Most authors advocate maintenance of skeletal fixation post-operatively for at least six weeks to allow healing of the soft tissues, followed by active range of motion.8,11,12,17
Carpometacarpal joint dislocations are uncommon, accounting for <1% of hand injuries, and require a high index of suspicion to diagnose.2 Careful physical exam and scrutiny of radiographs is essential, including evaluation of the metacarpal cascade lines.21 For cases where CMC dislocation or other carpal derangement is suspected, CT scan can elucidate the carpal anatomy and articular relationships.19,20 Closed reduction may be attempted in acute cases, but surgical treatment is often required due to the unstable nature of these injuries. Various techniques have been described, but we recommend protecting the reduction with a simple transverse K wire construct placed from the ulnar border of the hand.