Tibial Post Fracture in Revision Posterior Stabilized Total Knee Arthroplasty
Bryant Bonner, MD, Shaun S. Patel, MD, Jeffrey Lange, MD
The authors report no conflict of interest related to this work.
©2019 by The Orthopaedic Journal at Harvard Medical School
An estimated 5.2 million total knee arthroplasties (TKA) were performed in the United States between 2000 and 2010,1 representing the most commonly performed inpatient procedure. TKA utilization in the US more than doubled from 1999 to 2008 with 600,000 TKAs being performed in 2008, and the estimated 2010 prevalence of total knee replacement in the US was 1.52% (or 4.7 million individuals).2,3 The number of TKAs performed in the US is projected to increase by 143% by 2050, to almost 4 million annually.4,5 Among TKA designs, the posterior stabilized (PS) implant is one of the most successful and widely used.6,7
The posterior stabilized total knee replacement includes a tibial post that substitutes for the posterior cruciate ligament (PCL) and engages with a femoral component cam mechanism which allows for both stability and femoral rollback in knee flexion. Several potential complications have been associated with the cam-post mechanism, including patellar clunk syndrome,8 tibial post wear,9 cam-post dislocation,9 and tibial post fracture.9,10 Tibial post fracture is a rare but significant cause of morbidity, occurring at a rate of less than 1% after implantation of primary posterior stabilized total knee replacement.11
The diagnosis of tibial post fracture and treatment options are important for the practicing orthopaedic surgeon to consider. We present a case of a fractured tibial post and provide a review of the literature regarding diagnostic approach and treatment options. .
TAKE HOME POINTS
- Tibial post fracture in posterior stabilized total knee arthroplasty is rare.
- Proposed mechanisms include excessive femoral component flexion and/or posterior tibial slope, posterior placement of the femoral component, anterior placement of the tibial tray, deep knee flexion.
- There is no clear consensus on definitive treatment for tibial post fracture, but the most common approach is polyethylene liner exchange.
LEVEL OF EVIDENCE Level V Case Report
KEYWORDSArthoplasty, knee, arthritis, revision, replacement, total knee replacement
A 67-year-old female with history of multiple right knee surgeries presented to our hospital with increased knee pain and instability approximately 3 weeks after hearing a “crunch” in her knee while getting dressed. She initially underwent a right primary total knee arthroplasty (TKA) in October 2002 for osteoarthritis with a posterior stabilized TKA, including an oxidized zirconium femoral component (Genesis II, Smith and Nephew, Memphis, TN). This was complicated by rupture of the quadriceps tendon in March 2003 for which she underwent primary repair. In April 2003, dehiscence of the wound occurred with failure of the quadriceps tendon repair. Irrigation and debridement with polyethylene exchange as well as revision quadriceps tendon repair was performed. In June 2004, the quadriceps tendon re-ruptured, and revision repair was undertaken using an Achilles allograft. In June 2005, another re-rupture of the quadriceps tendon occurred, and reconstruction of the extensor mechanism was undertaken using an unknown allograft. After this last procedure, and for the past 12 years prior to presentation, she had been doing well, ambulating with a cane, and living actively with no pain.
Upon presentation to our hospital in February 2017, physical examination revealed a well-healed anterior knee incision with no surrounding erythema, warmth, or induration. She was noted to have a moderate knee effusion with tenderness over the anterior knee. It was difficult to assess her coronal or sagittal stability given significant pain and guarding on exam. She was neurovascularly intact with a functioning extensor mechanism and no extensor lag.
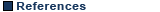
X-rays were notable for posterior subluxation of the tibia as well as a tibial component that was in varus alignment (Figure 1). There was concern for potential medial or lateral collateral ligament injury given her subjective instability, so further imaging was ordered. MRI revealed a fractured tibial post located in the suprapatellar pouch (Figure 2). Notable labs on admission included a white blood cell count of 7.32 K/uL (reference range 4-10 K/uL), erythrocyte sedimentation rate (ESR) of 53 mm/h (reference range 0-18 mm/H) and c-reactive protein (CRP) of 6.3 mg/L (reference range 0-3 mg/L). Given her elevated inflammatory markers, her knee was aspirated with 1800 nucleated cells (86% polymorphonuclear leukocytes) with a negative gram stain and negative culture that was followed for 14 days. Using shared decision making and after discussing the risks and benefits of surgical intervention, she opted to proceed with a revision right total knee arthroplasty.

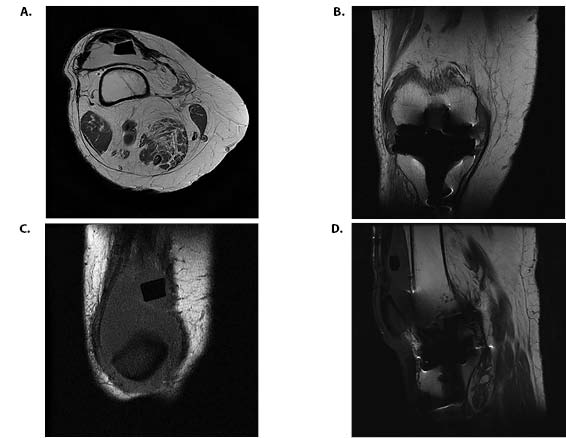
Revision surgery was carried out using standard medial parapatellar arthrotomy. The tibial post was noted to be fractured and buried within the femoral box (Figure 3). The post and the polyethylene insert were removed. The polyethylene insert was noted to have evidence of mild polyethylene wear. Inspection with a drop rod confirmed significant varus tibial baseplate alignment. The femoral component was inspected and found to be well fixed and undamaged. The decision was made to proceed with revision of the tibial component. The component and all cement was removed, and the tibia was recut to correct her previous varus alignment utilizing an intramedullary guide. A tibial baseplate with 15 mm medial and lateral augments and a 160 mm press-fit, offset stem was found to be satisfactory. A 15 mm ultra high molecular weight polyethylene (UHMWPE) insert was found to provide satisfactory range of motion and stability. The final components were assembled and inserted in usual fashion. Antibiotic-loaded cement (Simplex Bone Cement with Tobramycin, Stryker, Kalamazoo, MI) was utilized at the proximal tibia and stem-coupler interface. After implantation, the knee was stable to varus, valgus, anterior, and posterior stress; range of motion was estimated at 0-115 degrees; and patellar tracking was midline.

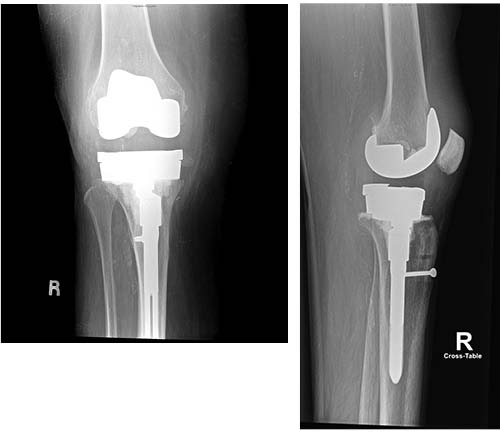
At six week follow-up, the patient was doing well and had returned home from rehab. She was using a walker for ambulation and could walk over 250 feet at a time. She was noted to have a 5 degree extensor lag, and her flexion was estimated at 120 degrees. She was most recently seen in March 2019–approximately 2 years out from her revision procedure–after a recent fall. She had no apparent hardware complication (Figure 4) and was wearing a neoprene knee sleeve for comfort.
Posterior stabilized TKAs are commonly used for TKA worldwide. Tibial post fracture is a rare but significant complication following PS TKA, occurring less than 1% of the time.11-13 It can lead to significant functional problems, including pain and instability, in patients who previously had a well functioning total knee arthroplasty.14 Susceptibility of the tibial post to fracture results from wear and deformation over time. Predisposing factors to post failure include excessive femoral component flexion, excessive posterior tibial slope, posterior placement of the femoral component, anterior placement of the tibial tray, and very deep knee flexion.11,13,15
The reported incidence of tibial post fracture in total knee arthroplasty widely varies. Hendel et al. reported an incidence of 1.2% in 332 patients over a five year period.15 Lachiewicz et al. reported an incidence of just 1 patient out of 193 (0.51%) over a 5 to 14 year follow-up period.13 Bal et al. reported the highest incidence of tibial post failure requiring revision with 70 out of 564 patients (12.4%). The implant studied, Foundation-100 Series Total Knee System – Encore Orthopedics, was noted to have a suboptimal tibial post design that had a central hole in the post for screw fixation of the tibial liner to the tibial tray, diminishing the post’s durability.16 In addition, it should be noted that many posts will show evidence of wear and deformation even in the absence of fracture. One study of four PS total knee arthroplasty designs looking at 23 posterior stabilizing polyethylene posts demonstrated that 40% of the tibial post surface revealed signs of deformation, and 30% had severe damage defined as a gross loss of polyethylene.17
While treatment decisions for tibial post fracture are made on a case by case basis, the most common treatment has been polyethylene liner exchange to a liner of increased thickness.11 Bal et al. demonstrated good short-term results in 18 knees following polyethylene exchange for this problem.9 Other authors have noted that revision of components, including conversion to a more constrained prosthesis for persistent varus/valgus and/or rotational instability after revision of the polyethylene insert, can produce good short term results in select cases.12,18
The etiology of post fracture for the patient presented here remains unknown. The patient had been doing well nearly 12 years after her last revision surgery. Her injury was atraumatic. It is notable that the tibial component was found to be in significant varus alignment upon presentation. It is unclear if it was initially placed in varus alignment at the index procedure or underwent loosening and subsidence into varus. As a result of its malalignment, the decision was made to revise the tibial component. While there have been no described reports of tibial post failure due to varus alignment, malalignment may have contributed to implant failure by producing abnormal stresses on the tibial post. Component alignment should be considered in this setting in order to optimize mechanics of the PS TKA and help improve implant survival and patient reported outcomes.19,20
Another potential risk factor for post failure may be related to the material properties of specific polyethylene inserts. Cross-linking polyethylene increases the resistance to adhesive and abrasive wear but results in decreased toughness, durability, and resistance to fatigue.21 More highly cross-linked polyethylene could be more prone to cracking based on increased brittleness.22-24 However, recent data suggests there is no significant difference in osteolysis, aseptic loosening, or polyethylene failure between TKAs that utilize highly crosslinked or conventional polyethylene.25-27 In the case presented here, however, highly cross linked polyethylene liners were not available from the manufacturer at the time of the initial TKA.
In summary, tibial post fracture following PS TKA is a rare, but significant, complication. In most cases, isolated polyethylene exchange is a successful solution; however more extensive revision surgery may be required in certain cases depending on the overall condition of the prosthesis.