Intramedullary Screw Fixation of Jones Fracture: The Crucial Starting Point and Minimizing Complications
Michael Aynardi, MD, Kempland C. Walley BS, and Jacob M. Wisbeck, MD
The authors report no conflict of interest related to this work.
©2019 by The Orthopaedic Journal at Harvard Medical School
Intramedullary screw fixation of the fifth metatarsal for metaphyseal-diaphyseal and diaphyseal fractures results in improved time to bony union, faster return to sport, and lower rates of repeat fracture compared to nonoperative treatment with immobilization. Although excellent outcomes have been described, complications may still occur.
In this technical tip, the authors present a technique for reproducibly achieving the correct entry point for intramedullary screw fixation of a Jones Fracture, facilitating proper trajectory during guidewire insertion, and safely guiding wire passage in cases of a sclerotic fracture site.
LEVEL OF EVIDENCE Level V Expert Opinion
KEYWORDSJones fracture, fifth metatarsal fracture, intramedullary screw fixation, foot fracture, surgical complications, foot surgery technique
Intramedullary screw fixation of the fifth metatarsal for metaphyseal-diaphyseal and diaphyseal fractures results in improved time to union, faster return to sport, and lower rates of repeat fracture compared to nonoperative management with immobilization.2,3,7,11,13 For these reasons, this technique has become the standard of care when these fractures are treated surgically.
Although excellent outcomes have been described,2 complications still occur. Nonunion, refracture, symptomatic hardware, and sural nerve injury are the most frequent complications following intramedullary screw fixation.4,6,15 Authors have described several techniques to minimize the risk of these complications including the utilization of larger diameter screws, passage of threads distal to the fracture site, percutaneous placement of pointed reduction forceps, and ensuring the proper entry point with correct trajectory within the medullary canal.3,10,13
A commonly cited technical article describes the “high and inside” guidewire starting point for optimal screw positioning.7,10 While the “high and inside” mantra is often repeated to orthopaedic trainees, achieving this position may still be difficult. Improper entry can result in refracture, delayed union or non-union,6,15 or surgical injury to the lateral dorsal cutaneous nerve.5
It is important to appreciate certain osseous characteristics—specifically the size, shape, and cortical quality—when performing surgical fixation of the fifth metatarsal. Failure to note the natural curvature of the bone may impede guidewire placement and lead to intraoperative complications. The width of the canal should be measured on the anteroposterior (AP) view of the foot, as the oblique image may lead to overestimation of the canal width. Improper measurement may result in compromise of the lateral cortex by the screw or drill and may precipitate fracture development. In addition, the fracture site may be sclerotic, depending upon the timing of injury and etiology of the fracture. Sclerosis can make passage of the guidewire difficult. In this clinical tip, the authors present a technique for reproducibly achieving the correct entry point for the guidewire, facilitating proper trajectory during guidewire insertion, and safely guiding the passage of the wire in cases of a sclerotic fracture site.
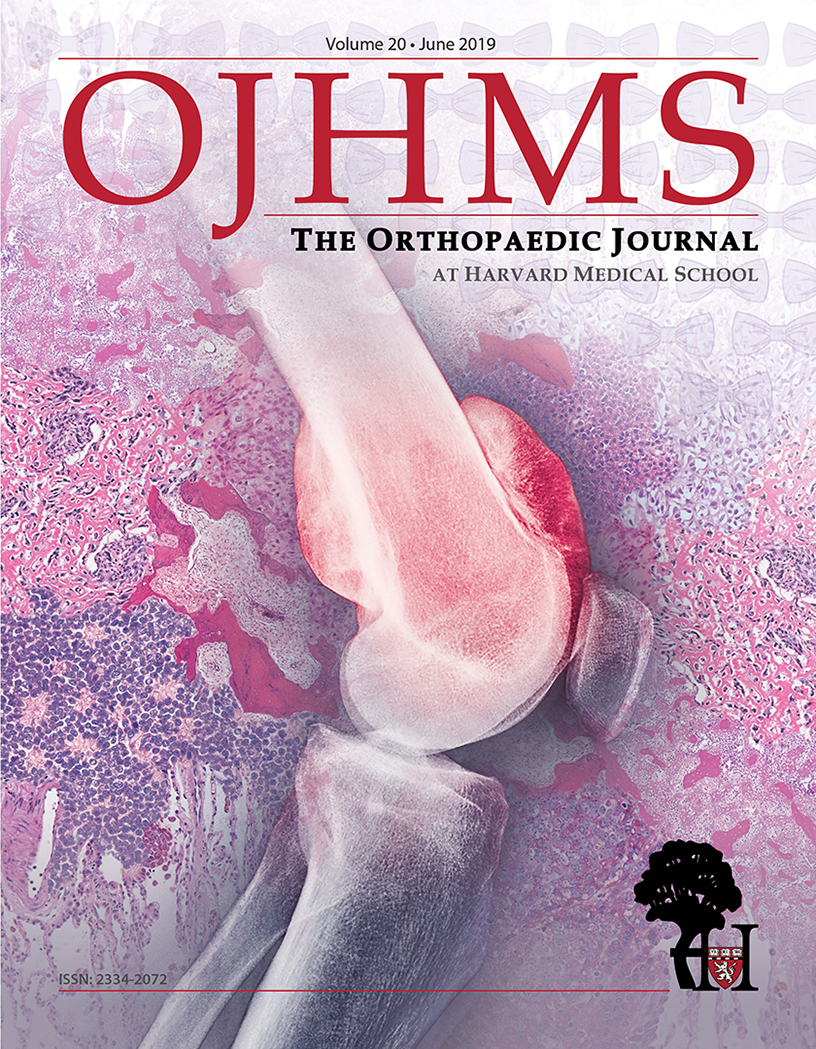
The authors generally perform fixation of fifth metatarsal fractures without the use of tourniquet as the tourniquet can precipitate ischemia to tissues, muscular injury, leg pain, neurovascular injury, and postoperative bleeding.1,8,9,12,14 However, surgeons may elect to utilize a tourniquet in order to improve visualization. After prepping and draping, the foot is positioned on the C-arm and a true AP image is obtained. The guidewire is placed over the center of the intramedullary canal and marked on the skin. It is important to note that the intramedullary canal of the fifth metatarsal is more medial than it appears on surface anatomy. Pressing the wire against the foot may help to achieve appropriate alignment (Figure 1A).
Many technical descriptions emphasize establishing the position of the guidewire on the oblique view.7 However, the authors recommend against the use of the oblique view for this purpose. The canal is narrowest on the AP imaging, and this measurement is representative of the true width of the canal. A lateral radiograph is then performed, and the guidewire is centered on the fifth metatarsal with its trajectory marked on the skin. Ensuring that the guidewire is centered on the AP and lateral views is paramount for achieving the correct trajectory of the screw.
At this point, there are two lines drawn on the skin. Next, the lateral view is used to mark a point 1 cm proximal to the fifth metatarsal base, and a 1-cm skin incision is made proximally to this mark but along the lateral line. This incision ensures that soft tissue will not resist guidewire positioning. Blunt dissection is utilized to protect the peroneus brevis and sural nerve (Figure 1A-E).
The guidewire is inserted utilizing the AP view of the foot as the surgeon and assistant ensure that the path of the guidewire is paralleling the lines drawn. Depending on patient anatomy, it may be beneficial to freehand the wire onto the start point because the lateral foot may impede optimal positioning of the wire driver (Figure 1E). Radiographs are performed to ensure a central location in the AP and lateral views. The wire should be driven up to but not past the fifth metatarsal curvature to avoid risk of cortical penetration.
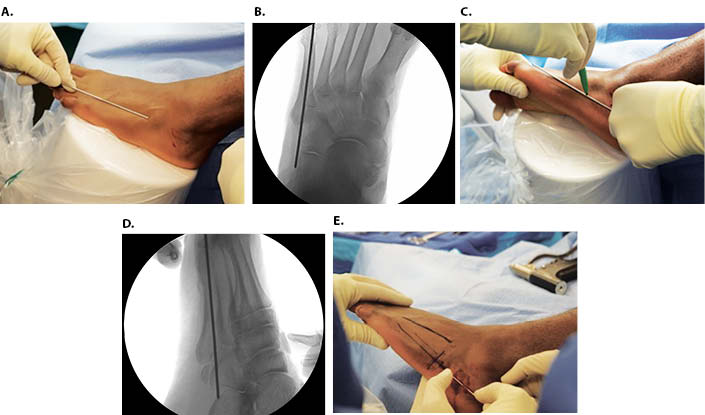
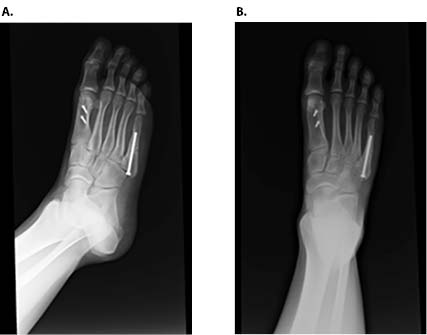
The use of a freehand drilling technique can aid in passing the guidewire beyond a sclerotic fracture site while ensuring that the wire passes centrally within the fifth metatarsal canal. For this technique, the start point is determined as previously described. However, the guidewire is only inserted far enough to obtain the start point but not engage the sclerotic bone. Under fluoroscopy, the drill is advanced along the proper trajectory up to and across the fracture site, opening the canal (Figure 2). The guidewire is then inserted through the drill and safely beyond the fracture site (Figure 3). Its position is confirmed on two fluoroscopic views, and the screw is measured, tapped, and inserted (Figures 4 and 5).



Intramedullary fixation of Jones’ fractures can result in improved patient outcomes in athletic populations,2,6,11 but avoiding complications is paramount. The majority of intraoperative complications result, either directly or indirectly, from improper starting point and poor screw trajectory.7 The technical pearls in this article have helped the authors to avoid these complications, and these techniques may result in improved component alignment, decreased surgical time, and improved surgical technique for resident and fellow orthopaedic trainees.