Musculotendinous Junction Tears of the Subscapularis: A Report of Two Cases
Stuart D. Kinsella, MD, MS, Sean Michael Rider, MD, Emily M. Brook, BA, Jon J.P. Warner, MD, Elizabeth G. Matzkin, MD
The authors report no conflict of interest related to this work.
©2017 by The Orthopaedic Journal at Harvard Medical School
OBJECTIVE Tears of the subscapularis at the musculotendinous junction are rare and underreported in the literature.
METHODS We report the cases of two young and active patients, a 28-year-old female and a 48-year-old male, who presented with persistent shoulder pain. Imaging studies (MRI) revealed incomplete tears at the musculotendinous junction of the subscapularis without other significant rotator cuff pathology.
RESULTS One patient was managed conservatively with formal physical therapy and NSAIDs, and was able to return to full activity. The second patient underwent an arthroscopic procedure, yet no intervention to the subscapularis was performed, as the musculotendinous junction was not readily visualized using standard arthroscopic technique. The patient was subsequently managed with conservative treatment modalities and was able to return to activity.
CONCLUSION This case series on musculotendinous junction tears of the subscapularis highlights the difficulty of diagnosis and limitations of surgical intervention using standard arthroscopic technique. Our experience suggests that this uncommon injury may be successfully managed with conservative treatment modalities such as cryotherapy, NSAIDs, and physical therapy.
LEVEL OF EVIDENCE Therapeutic Level IV, Case report
KEYWORDS musculotendinous junction, rotator cuff, subscapularis, shoulder, upper extremity
The subscapularis is the largest and most powerful rotator cuff muscle.1 Isolated injuries to the subscapularis tendon are rare and often secondary to trauma in a young and active population.2-4 Subscapularis injuries can result in significant pain and weakness, but remain difficult to clinically diagnose, with previous literature indicating low sensitivity of the lift-off and belly-press tests.5-10 A thorough physical examination is important to raise suspicion for any rotator cuff pathology, however, current examination techniques are limited in their ability to accurately diagnose subscapularis tears.
In addition, subscapularis tendon pathology can be difficult to diagnose under arthroscopy, as only the superior and superolateral margins of the tendon are readily visualized with the use of standard portals, specifically the standard posterior portal.11 Given the difficulty of diagnosis under arthroscopy, significant attention has been directed towards diagnostic imaging modalities that can provide adequate visualization of the subscapularis. Magnetic Resonance Imaging (MRI) has been the gold standard of imaging studies for the analysis of soft tissue shoulder pathology.12 A recent investigation comparing MRI and arthroscopic findings in patients with injury to the subscapularis concluded that MRI can be used to accurately evaluate subscapularis pathology despite some limitations.13
Rotator cuff injuries at the musculotendinous (MT) junction are distinct from tendon injuries in regards to anatomic location, pathophysiology, and prognosis.14,15 Furthermore, a recent investigation of MRI findings found no correlation between the presence of MT junction injury and tendon injury.16 In addition, the study found that 25% of subscapularis tears were localized to the MT junction.16
We present the cases of two young and active patients with tears to the MT junction of the subscapularis, highlighting the difficulty of clinical diagnosis, visualization on diagnostic imaging and under arthroscopy, and the implications of decision making for treatment modalities.
Case 1
A 28-year-old female police officer and paramedic presented to our clinic with 5 months of right shoulder pain. The pain began after she lifted herself off the ground using a rope at the gym. She felt a “pop” in the right shoulder, immediate warmth, and pain from the shoulder radiating down into the biceps and the right side of her chest. She first presented to her primary care physician who then referred her to a local orthopedist, where initial plain radiographs were obtained and demonstrated no fracture, dislocation, or bony injury. A corticosteroid injection to the shoulder, not further specified, was attempted as a conservative treatment modality, but resulted in minimal relief. Following this, an MRI was ordered and demonstrated mild edema and a possible partial tear of the right subscapularis tendon. The patient subsequently presented to our clinic for repeat evaluation of her persistent right shoulder pain. The patient’s past medical and surgical history, medications, and allergies were unremarkable, and she was otherwise healthy.
On physical examination, she was able to perform overhead activities without significant pain, however, any activities involving movement behind her back or cross-chest exercises exacerbated pain localized to the anterior aspect of the shoulder. On examination, she had positive lift-off, bear-hug, and belly-press signs. She had full range motion and strength of her deltoid, supraspinatus, and infraspinatus muscles but exhibited weakness with internal rotation strength testing with the arm in adduction. Suspicion for labral pathology was raised in part due to a positive O’Brien’s test in the context of the patient’s history, though O’Brien’s can be associated with several other shoulder pathologies. Speed’s and Yergason’s tests were negative. She was tender to palpation over the anterior shoulder and coracoid process and was otherwise neurovascularly intact.
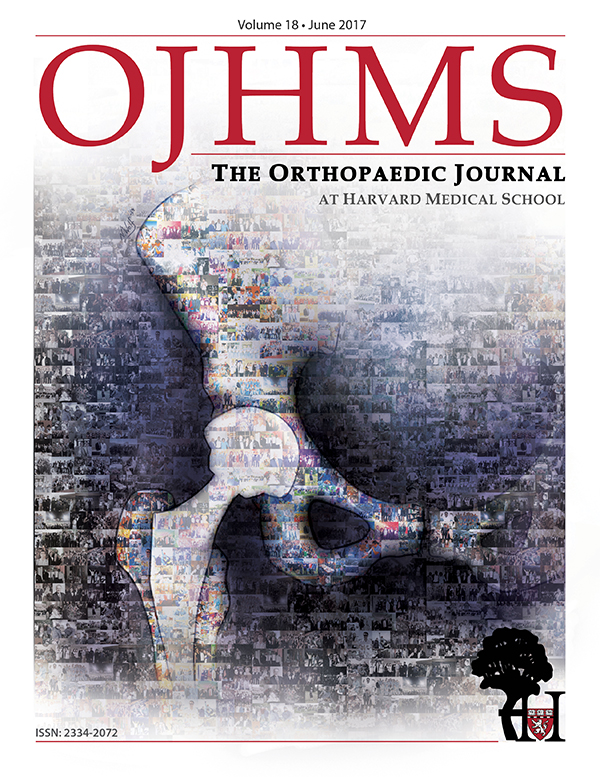
Given the poor quality of her initial MRI and the suspicion for labral pathology, an MRI arthrogram was ordered. At follow-up two weeks later, the patient’s pain was minimally improved, with no changes to her physical examination. The MR arthrogram demonstrated a partial thickness tear of the subscapularis at the MT junction, in addition to supraspinatus tendinosis (Figure 1).
(A) T2 Axial (B) T2 Coronal and (C) T2 Sagittal
Conservative treatment modalities were prescribed including activity modification, NSAIDs, and a course of formal physical therapy. She was able to return to moderate weight lifting activities 3 months after initial presentation to our clinic, although she continued to be mildly limited by pain during internal rotation maneuvers. Nine months after her initial onset of pain, she had full active and passive range of motion, as well as full strength of the subscapularis with negative bear hug, belly-press, and lift-off signs. She gradually progressed to full weight lifting activities, and her only residual symptoms were occasional nighttime soreness one year after her initial onset of symptoms.
Case 2
A 48-year-old male competitive weightlifter presented to our clinic with three months of left shoulder discomfort. Though there was no known traumatic injury, the patient noticed increasing pain and discomfort with certain overhead weightlifting maneuvers, especially those requiring internal rotation. The patient’s past medical and surgical history, medications, and allergies were all reviewed and found unremarkable and he was otherwise healthy.
On physical examination, there was no obvious atrophy or asymmetry of his shoulders, and he was neurovascularly intact. He had full range of motion and positive lift-off and belly-press signs. He exhibited weakness with internal rotation, with hand-held dynamometry measurements demonstrating 8.8kg on the left side compared to 15.2kg on the contralateral side. In addition, Speed’s and O’Brien tests were positive without any tenderness in the bicipital grove.
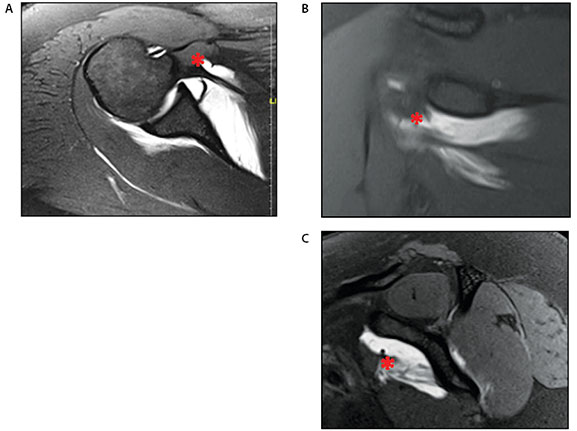
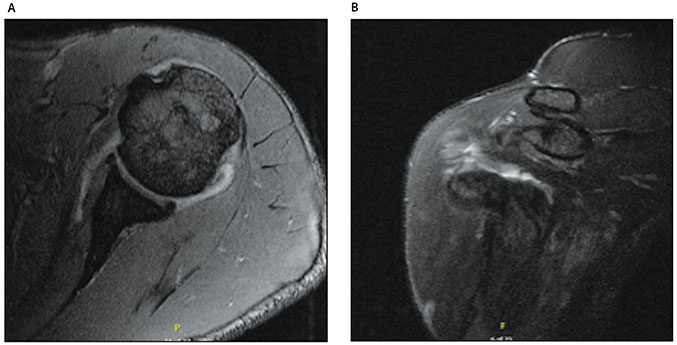
An MRI was subsequently performed, and revealed a small tear at the anterior leading edge of the supraspinatus, as well as a tear of the subscapularis at the MT junction with minimal loss of subscapularis bulk (Figure 2). There was no significant biceps pathology.
(A) T2 axial and (B) T2 coronal
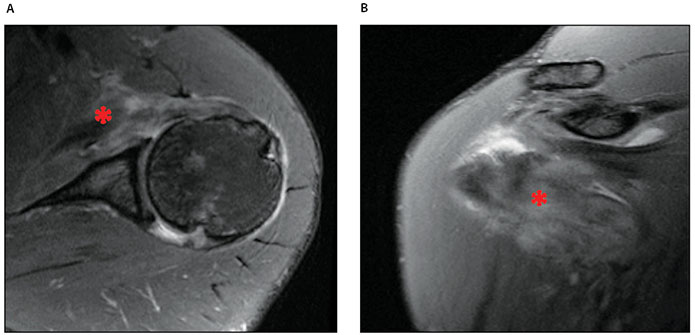
The patient had minimal improvement after three months of conservative treatment modalities and elected to undergo arthroscopic intervention for further evaluation. Intra-operative findings were significant for mild articular sided supraspinatus fraying and inflammation surrounding the biceps tendon. Thorough arthroscopic evaluation demonstrated no evidence of subscapularis tear (Figure 3). The tendon was probed to the level of conjoined tendon and the coracoid, and visualized through the rotator interval to the beginning of the MT junction. While mild inflammation of the subscapularis was noted, there was no clear structural disruption. The subacromial space contained thickened and inflamed bursal tissue. An arthroscopic subacromial decompression and biceps tenodesis was performed without any intervention to the subscapularis.
Significant findings were (A) inflammation surrounding the biceps tendon and (B-D) demonstrating an inflamed subscapularis tendon without clear structural disruption.
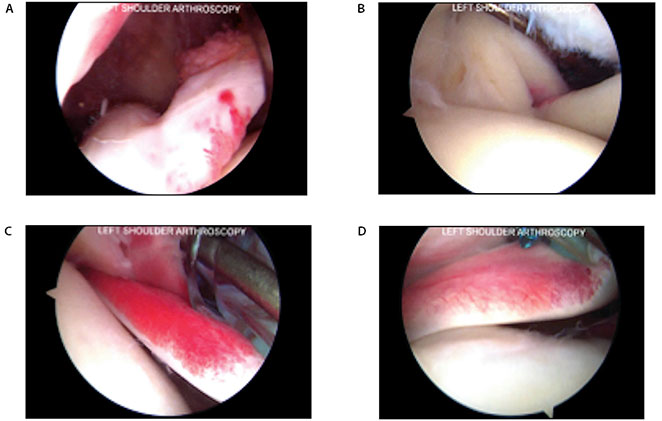
Approximately four months after the arthroscopic procedure and seven months from the initial onset of symptoms, the patient returned to clinic reporting persistent weakness specific to internal rotation weightlifting maneuvers. A follow-up MRI was obtained and demonstrated some healing of the subscapularis MT junction tear (Figure 4). Physical examination was notable for weak, but improved internal rotation strength, measured at 12kg on the left compared with 16kg on the right side. Despite persistent weakness with internal rotation, the patient reported minimal discomfort in daily activities and a steady improvement in his weightlifting activity. Given the risks and long rehabilitation of an open subscapularis repair, a decision was made to pursue conservative treatment measures. At last follow-up five months following the arthroscopic procedure and eight months from the initial onset of symptoms, the patient continued to improve with physical therapy. He was instructed to return to clinic if his symptoms returned or he was unable to return to his prior activity level.
(A) T2 axial and (B)T2 coronal
Historically, subscapularis tears were thought to be uncommon but recent studies have demonstrated that subscapularis tendon tears have been observed in up to 30% of shoulder arthroscopies and 49% of rotator cuff surgeries.10,17,18 One reason for the paucity of literature on subscapularis pathology relative to other rotator cuff pathology is the difficulty in diagnosis, attributable to the unique anatomy of the subscapularis tendon.19 In a retrospective study of 348 arthroscopic rotator cuff repairs comparing MRI and arthroscopic findings of subscapularis tears, MRI sensitivity for subscapularis tendon tears was only 25%.20 Another study showed that MR arthrogram does not offer substantial improvement in the sensitivity of diagnosing subscapularis tendon injury, with a sensitivity of 36%.21
Current literature indicates that both arthroscopy and MR imaging can be inaccurate in the diagnosis of injury to the MT junction of the subscapularis. Therefore, a better understanding of the anatomy of the subscapularis at the MT junction is necessary to improve diagnosis of potential pathology. The superior portion of the subscapularis becomes tendinous at the level of the glenoid and has a broad footprint on the lesser tuberosity.22 In a cadaveric study of the anatomy of the subscapularis tendon and MT junction, the subscapularis muscle was found to insert on the humerus as both tendon and muscle. Notably, the superior 60% of the muscle’s insertion was tendinous, while the remaining 40% was muscle below the lesser tuberosity, which further impedes arthroscopic evaluation of the MT junction.23 The second case presented highlights the difficulty in visualizing the MT junction under arthroscopy.
Musculotendinous rotator cuff injuries of the supraspinatus and infraspinatus have received greater attention in the literature and may provide insight into the diagnosis and treatment for subscapularis MT pathology. Supraspinatus rupture at the MT junction is rare, but has been previously reported. One report of a supraspinatus rupture at the MT junction demonstrated good clinical outcome with non-operative treatment.24 A case series of five patients with supraspinatus ruptures at the MT junction found increased edema on T2 sequences of the MRI, similar to the findings in our cases. In addition, the authors reported that non-operative treatment modalities were more successful for incomplete MT junction tears compared to complete tears.14 Two recent case series have highlighted infraspinatus MT injuries and found no difference in clinical outcome between operative and non-operative treatment.15,25
In our cases, one patient had success with non-operative treatment modalities such as physical therapy and was able to return to full activity. Although the second patient underwent arthroscopic intervention after failing initial conservative treatment measures, the subscapularis injury at the MT junction was not specifically addressed. One can speculate that with longer conservative management, the outcome may have been similar to the first patient. This case highlights the discordance between MRI findings and arthroscopic findings, as the MRI confirmed diagnosis of a subscapularis rupture at the MT junction, yet the tear was not visualized under arthroscopy due to the anatomic location of the MT junction with the use of standard portals.26 As a result of the difficulty in arthroscopic assessment of the subscapularis, there has been heighted attention towards improvements in arthroscopic technique that might allow for more comprehensive evaluation.27-29 Greater study of MT junction tears in epidemiology, diagnosis, and treatment may allow for better classification of patients that may benefit from non-operative versus operative treatment modalities.
We present two cases of symptomatic tears at the MT junction of the subscapularis. Previous literature indicates that MT junction injuries to the subscapularis are rare, yet remain an important consideration in patients with suspected subscapularis pathology. The two case presentations highlight the importance of a thorough physical examination and the potential conflicting findings between MRI and arthroscopic evaluation of the MT junction of the subscapularis. Both patients demonstrated clinical improvement without operative intervention to the MT subscapularis tear over a minimum of 6 months. This uncommon injury may be successfully managed with non-operative treatment including cryotherapy, NSAIDs, and physical therapy.