Variation in Orthopaedic Trauma Management between Haitian and American Orthopaedic Surgeons
Heather J. Roberts, MD, Abhiram R. Bhashyam, MD, MPP, Rameez A. Qudsi, MD, George S. M. Dyer, MD
The authors report no conflict of interest related to this work.
©2017 by The Orthopaedic Journal at Harvard Medical School
OBJECTIVE The burden of disease from orthopaedic trauma is growing in low- and middle-income countries, such as Haiti. While orthopaedic outcomes differ between Haiti and the United States, it is unknown if these differences are due to variation in surgical training, resource availability, or other factors. The aim of this study was to understand how and why management of orthopaedic trauma conditions varies between Haitian and American surgeons.
METHODS Using an audience response system, we surveyed 49 Haitian and 41 American orthopaedic attending surgeons and residents to assess management of eight common orthopaedic trauma cases: mid-shaft femur fracture, mid-shaft tibia fracture, distal femur fracture, posterior acetabular wall fracture, femoral neck fracture in a young patient, femoral neck fracture in an elderly patient, glenoid fracture dislocation, and bimalleolar ankle fracture. Participants selected the one treatment they would choose to manage each case in their hospital from a provided list. Each case management question was followed by a multiple-choice question asking why a proposed management option was not selected. The Chi-squared statistic was used to detect differences in response distribution between Haitian and American respondents.
RESULTS There was no significant difference in management of femoral shaft fractures (p=0.66). Haitians were more likely than Americans to cast a mid-shaft tibia fracture (49% vs. 13%, p=0.008). The reasons Haitians cited for not using an intramedullary nail were complications (30%) and implant requirements (20%). Haitians were less likely than Americans to use a condylar locking compression plate for a distal femur fracture (49% vs. 87%, p=0.048) due to limited implant availability (50%) and perceived worse functional outcomes (40%). Haitians were less likely than Americans to use open reduction and internal fixation for an acetabular fracture (63% vs. 95%, p=0.016) due to low confidence (36%) and resource limitations (43%) associated with operative intervention. Haitians chose options other than arthroscopy for a glenoid fracture repair due to low confidence (23%) and resource limitations (74%) associated with arthroscopic stabilization.
CONCLUSION This survey demonstrates that for conditions that are managed differently in Haiti than in the U.S., the treatment rationale in Haiti is context-specific. The management of complex conditions, such as acetabular fractures, is limited by training, while the management of common conditions, such as mid-shaft tibia fractures, is influenced by the prevalence of complications and implant availability. This highlights the need for targeted, context-specific interventions that include resource allocation and associated education around the use of those resources.
LEVEL OF EVIDENCE Level IV, Cross sectional survey
KEYWORDS Global orthopedics, orthopedic trauma, education, low-income country
Musculoskeletal trauma is a growing source of morbidity and mortality in developing countries. According to a 2002 report, an estimated 5 million people worldwide die annually from injuries, and 90% of those deaths occur in low- and middle-income countries (LMICs).1 In part due to rising rates of motor vehicle accidents, this number is likely higher today than in 2002.2 Orthopaedic injury and disease constitute 14% of the world’s disability adjusted life-years (DALYs) lost and 9% of the world’s mortality, according to WHO estimates.3
Outcomes for victims of trauma are worse in developing (low and low-to-middle income) countries than in developed, high-resource settings. According to one estimate, 34-38% of all injury deaths could be avoided if trauma in low-resource countries was managed as it is in high-income countries.4 This discrepancy is likely multifactorial, including severity of injury, patient comorbidities, timing of presentation, physician training, and resource availability. To our knowledge, no prior studies have compared the decision-making process behind management of orthopaedic trauma between orthopedic surgeons in low- and high-income countries. An understanding of such differences, along with needs assessments of surgeons in low-income countries, may allow for more targeted resource allocation and thereby improvement in trauma care.
The purposes of this study were to understand how management of eight orthopaedic injuries varies between Haitian and American orthopaedic surgeons and to begin to explore the reasons behind that variation. We hypothesized that management variation depends on the case, with resource availability being the primary reason for management variation.
We performed a survey of practicing orthopaedic surgeons and residents regarding their treatment preferences and decision-making processes as they relate to orthopaedic injuries. The study protocol was reviewed and approved by the institutional review board at the principal investigator’s hospital. A survey was designed to assess management of eight fractures: mid-shaft femur fracture, mid-shaft tibia fracture, distal femur fracture, posterior acetabular wall fracture, femoral neck fracture in a 30 year old patient, femoral neck fracture in an 80 year old patient, glenoid fracture dislocation, and bimalleolar ankle fracture. Respondents were asked to choose the one management option that they would use at their hospital, given the particular resource constraints of their practice environments. For each case, relevant demographic information and imaging was provided, and between three and eight answer options were listed. Questions and answer choices were refined with input from two independent, fellowship-trained attending American orthopaedic surgeons. Each case question was followed by a question to assess the rationale for choosing the previous management option. One management option was chosen as a reference for comparison, and each rationale question asked if the reference option was not chosen and why. Nine rationale answer choices were provided for each question to include a range of reasons, including level of training, outcome considerations, and resource limitations. Demographic information about respondents, including nationality, age, gender, years in practice, was also collected.
The survey was administered to Haitian and American orthopaedic residents and attending surgeons using the TurningPoint audience response system (Turning Technologies). Both resident and attending surgeons were surveyed to increase sample size. American orthopaedic residents from the principal investigator’s home institution were surveyed. Haitian orthopaedic residents and both Haitian and American orthopaedic attending surgeons were surveyed at an annual orthopaedic trauma conference in Port-au-Prince, Haiti. Participation was voluntary and anonymous.
Descriptive statistics for demographics of respondents were calculated. Pearson’s chi-squared test was used to detect differences in response distributions between Haitian and American respondents. The significance criteria was adjusted for multiple comparisons using the Bonferroni correction to α<0.0063. Statistical analysis was performed using Stata 13.1 software.
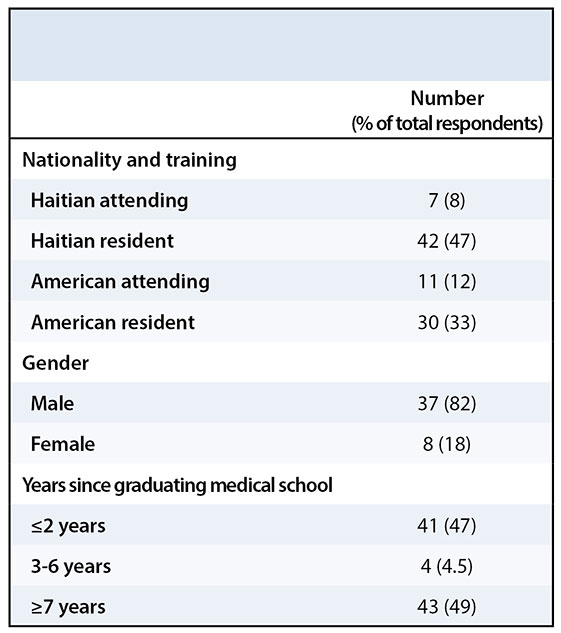
Survey respondents consisted of 49 Haitian and 41 American orthopaedic surgeons, and the survey response rate was 86%. Of the respondents, 80% were orthopaedic residents; 82% were male; and 51% had graduated from medical school ≤ 6 years ago (Table 1). Due to the low proportion of attending respondents, we were unable to perform a meaningful subgroup analysis comparing resident to attending responses.
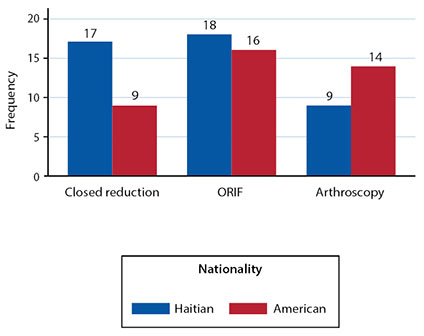
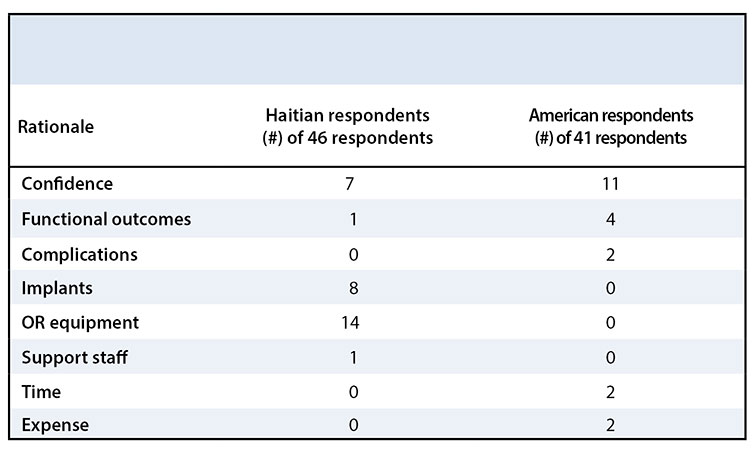
The response distribution for the management of each case varied across cases and nationality. Table 2 shows the modal answer for each case and the number of answer choices that were represented by at least one respondent, by nationality. There was no significant difference between Haitian and American orthopaedic surgeons in the management of a mid-shaft femur fracture, in which the most common management choice was an antegrade nail (p = 0.58); femoral neck fracture in a young patient, in which the most common management choice was open reduction and internal fixation (ORIF) (p = 0.47); femoral neck fracture in an elderly patient, in which the most common management choice was hemiarthroplasty among Haitian respondents and total hip arthroplasty among American respondents (p = 0.01, not significant after adjustment for multiple comparisons); bimalleolar ankle fracture, in which the most common management choice was ORIF of lateral and medial malleoli (p = 0.33); or glenoid fracture dislocation, in which the most common management choice was ORIF (p = 0.33). Regardless of nationality, there was little consensus about the management of a glenoid fracture with associated dislocation with all three answer choices highly represented (closed reduction, ORIF, and arthroscopic stabilization) (Figure 1). Haitians reported operating room equipment availability (n = 14/46), implant availability (n = 8/46), and confidence performing the operation (n = 7/46) as reasons not to perform arthroscopic stabilization. Americans reported confidence (n = 11/41), functional outcomes (n = 4/41), complications (n = 2/41), time (n = 2/41), and expense (n = 2/41) as the reasons not to perform arthroscopic stabilization (Table 3).
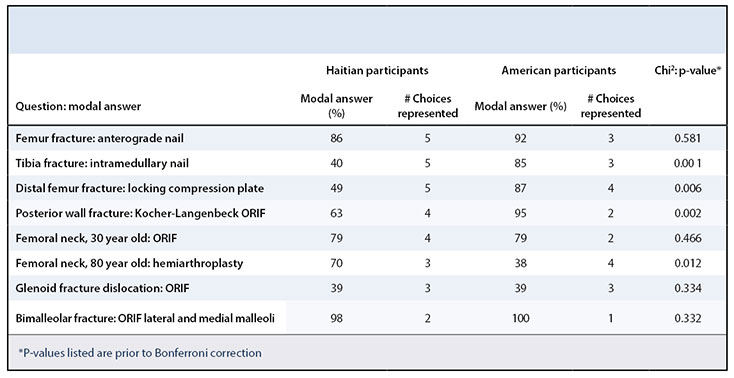
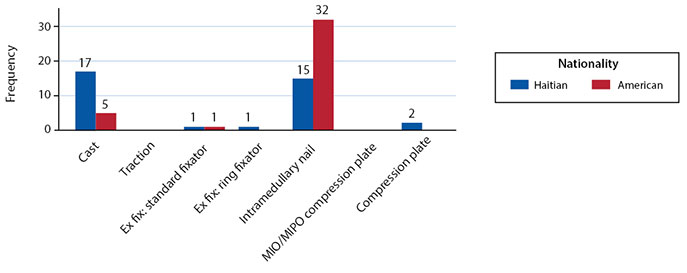
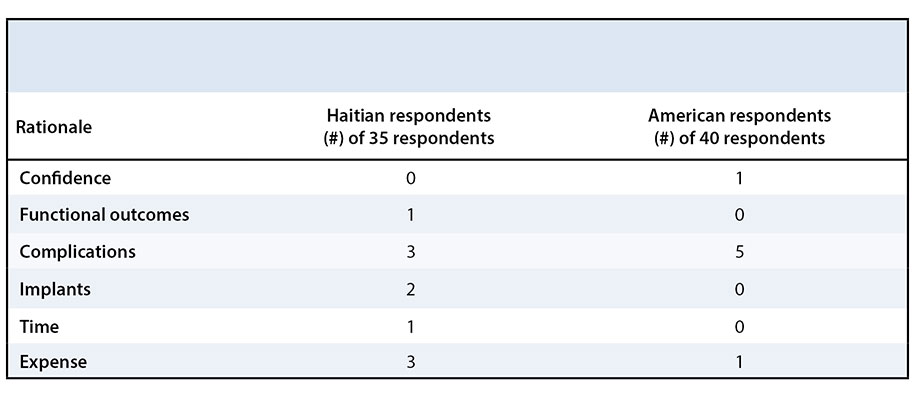
Haitians and Americans reported significantly different management of a mid-shaft tibia fracture (p = 0.001), with Haitians more likely to cast (n = 17/35) and Americans more likely to use an intramedullary nail (n = 34/40) (Figure 2). Haitians reported complications (n = 3/35), expense (n = 3/35), and implant availability (n = 2/35), while Americans reported confidence (n = 1/40), complications (n = 5/40), and expense (n = 1/40) as reasons not to use an intramedullary nail for a mid-shaft tibia fracture (Table 4).
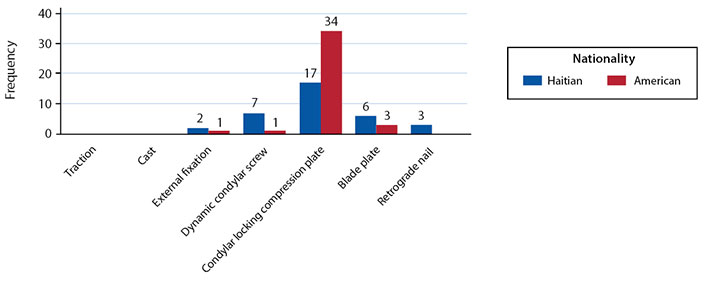
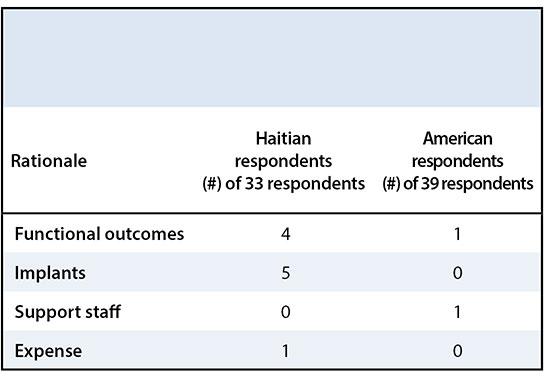
Americans were more likely to use a condylar locking compression plate for management of a distal femur fracture (n = 34/39), while condylar locking compression plate (n = 17/33), dynamic condylar screw (n = 7/33), and blade plate (n = 6/33) were highly represented among Haitian orthopaedic surgeons (p = 0.006) (Figure 3). Haitians reported implant availability (n = 5/33) and functional outcomes (n = 4/33), while Americans reported functional outcomes (n = 1/39) and support staff (n = 1/39), as reasons not to use a condylar locking compression plate for a distal femur fracture (Table 5).
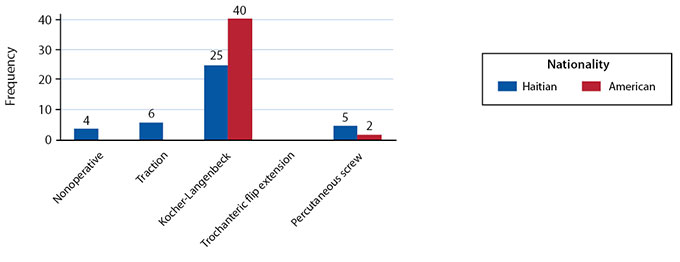
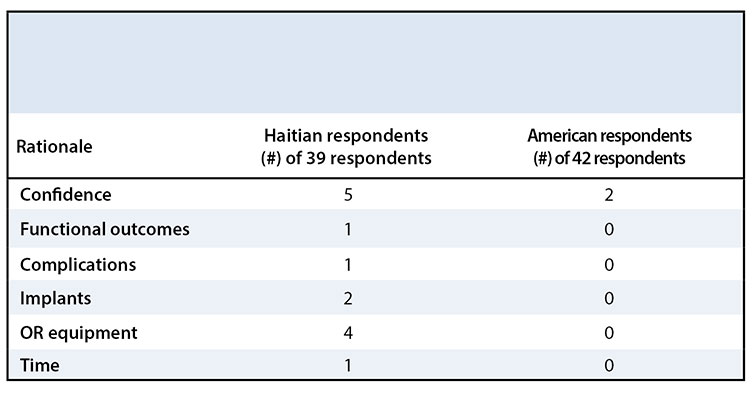
The majority of Americans chose ORIF for the management of a posterior hip dislocation with a displaced fracture of the posterior wall (n = 40/42), while Haitians chose ORIF (n = 25/39), non-operative management (n = 4/39), or skeletal traction (n = 6/39) (p = 0.002) (Figure 4). Haitians reported confidence performing the operation (n = 5), operating room equipment availability (n = 4), and implant availability (n = 2), while Americans reported confidence (n = 2), as reasons not to perform ORIF in this case (Table 6).
Regional variation in orthopaedic management across the United States has been documented for various conditions.5-8 Explanations for such variation may include differences in patient population or disease epidemiology; local effect of the environment in which a surgeon trains or practices; reimbursement schemes; or novelty of new technologies. Variation in orthopaedic surgeon decision-making between low- and high-income countries has not previously been explored. In this study, we show that the management of three common orthopaedic injuries varies between Haitian and American orthopaedic surgeons.
Four of the cases surveyed showed no difference in management, which suggests that many orthopaedic trauma cases are managed similarly across countries. Of the three cases with significantly different management strategies, implant availability was a frequently cited reason among Haitian surgeons for not choosing the reference response, which supports known resource constraints and diminished surgical infrastructure in Haiti.9 While the management options chosen for mid-shaft tibia fracture and distal femur fracture differed between Haitians and Americans, reported outcomes of the different management options are similar,10-16 suggesting that, despite resource limitations, differences in decision-making may not be clinically significant. While the burden of pelvic and acetabular injury is high in developing countries,17,18 surgery is uncommon in Haiti due to surgical training and equipment availability, such as C-arm, as reflected in this survey. The response to management of a glenoid fracture dislocation confirmed the anecdotal belief of reduced access to arthroscopic equipment and training in Haiti.
A recent study comparing orthopaedic operative volume between a hospital in Ghana and a hospital in the United States showed a disproportionate burden of trauma, severe fractures, and infections in Ghana as compared to the United States.19 Therefore, differences in patient demographics and injury severity likely contribute to differences in outcomes. Orthopaedic burden in Haiti has similarly high volumes of orthopaedic trauma and infections,20 which may influence surgeon decision-making as well as patient outcomes, though this was not evaluated in the current survey and would need to be explored further.6,12
This study has several limitations. First, the survey respondents may not represent orthopaedic surgeons as a whole in Haiti and the United States. Respondents were primarily orthopaedic surgery residents with few attending surgeons represented among our respondents. While residents are not ultimately responsible for choosing surgical management, their responses likely reflect the teaching they receive from attendings in their practice environment. Additionally, the American attendings surveyed were those who elected to travel to Haiti and therefore may not represent U.S. surgeons as a whole; however, as practicing orthopaedic traumatologists, they were experienced in the cases represented in this survey. Second, surgeons were surveyed about hypothetical cases, and their responses may not represent the management choices they would make in practice. A study of injury presentation and management to explore surgical decisions in practice would provide more detailed information about how management decisions differ between countries. Third, previous studies have shown that injury pattern and severity differs between low- and high-income countries;18,19,21 while these differences are likely to affect surgical management, they were not explored in this survey. Other factors that may influence management decisions, including timing between injury and presentation; patient ability to comply with planned treatment follow-up; access to specialists, critical care, and anesthesiology; and referral patterns, were not addressed in this survey.
These data, while limited by the high representation of residents and the limited scope of the survey design, provide preliminary evidence of the potential difference in management decisions surrounding orthopaedic trauma between Haitian and American orthopaedic surgeons. In particular, they suggest that implant availability and specialized orthopaedic trauma training in pelvic surgery and arthroscopy are current deficits in orthopaedic trauma care capacity in Haiti and may be areas of need for future study and development. As with the introduction of any new equipment, adequate training in its use is necessary to ensure appropriate implementation. Other infrastructure required for advanced trauma care, including general surgery; anesthesiology; radiology; and pharmacy, was not assessed in this survey but may represent additional needs that influence surgical decisions. Future studies should examine management of orthopaedic injuries in practice, rather than in a survey, to better characterize differences. These results could be used improve resource allocation to low-income settings such as Haiti.