|
Chairman's Corner: Introduction
 We had a very successful match again this year. As you
recall we are in the midst of expanding our program from 10
to 12 residents per year. (This increases our total number of
residents from 50 to 60.) With this recent match completed we
will have 12 residents through the PGY 4 year beginning July
1, 2006. The full conversion to 60 residents will occur after the
next match in July, 2007. This July with 12 residents in the
PGY 4 year we will begin our two-month research rotation (the
goals and objectives I described to you in last year’s Director’s
Corner). Every two months two residents will rotate on the service
and will have lectures, seminars, journal clubs, on-line and
reading requirements, as well as the opportunity to complete
their thesis work
We had a very successful match again this year. As you
recall we are in the midst of expanding our program from 10
to 12 residents per year. (This increases our total number of
residents from 50 to 60.) With this recent match completed we
will have 12 residents through the PGY 4 year beginning July
1, 2006. The full conversion to 60 residents will occur after the
next match in July, 2007. This July with 12 residents in the
PGY 4 year we will begin our two-month research rotation (the
goals and objectives I described to you in last year’s Director’s
Corner). Every two months two residents will rotate on the service
and will have lectures, seminars, journal clubs, on-line and
reading requirements, as well as the opportunity to complete
their thesis work
The Second Annual OREF New England Research
Symposium was held at the Massachusetts General Hospital
on May 5, 2006, which was hosted by Dempsey Springfield,
M.D. and myself. Fifteen papers were presented and three
awards were given. Residents from our program who presented
terrific papers included: Andrew Jawa, MD (“Extra-articular
distal-third diaphyseal fractures of the humerus: Comparison
of Functional Bracing and Plate Fixation”), Alexander Sah,
MD, (“Survival of the prosthesis beyond the patient: unicompartmental
knee arthroplasty in octogenarians”), and Nina
Shervin, MD, (“Hospital and surgeon procedure volume with
patient-centered outcomes of orthopaedic surgical procedures:
a systematic review of the literature”). The judges were: David
Ayers, MD (University of Massachusetts), Charles Cassidy, MD
(Tufts), James Heckman, MD (Editor, Journal of Bone and Joint
Surgery), Paul Hecht, MD (Dartmouth), Dempsey Springfield,
MD (Harvard), Richard Terek (Brown) and myself. The keynote
address was given by Kevin Bozic, MD, MBA entitled “Disruptive
Innovations in Orthopaedics.” Kevin’s talk was unique and
outstanding. I know he stimulated everyone into new ways
of thinking about introducing new technologies and our very
dysfunctional health care system.
We continue to assess our residents as required by the
ACGME in the six Core Competencies. I thought you might be
interested to see how we are doing as a residency program measuring
the outcomes of these educational efforts. An accurate
measurement of the effectiveness or outcomes of our teaching
program is the eventual goal for each competency required by
the ACGME. This is a list of our methods to evaluate the residents
in each of the six Core Competencies: (those with * are
measurement tools)
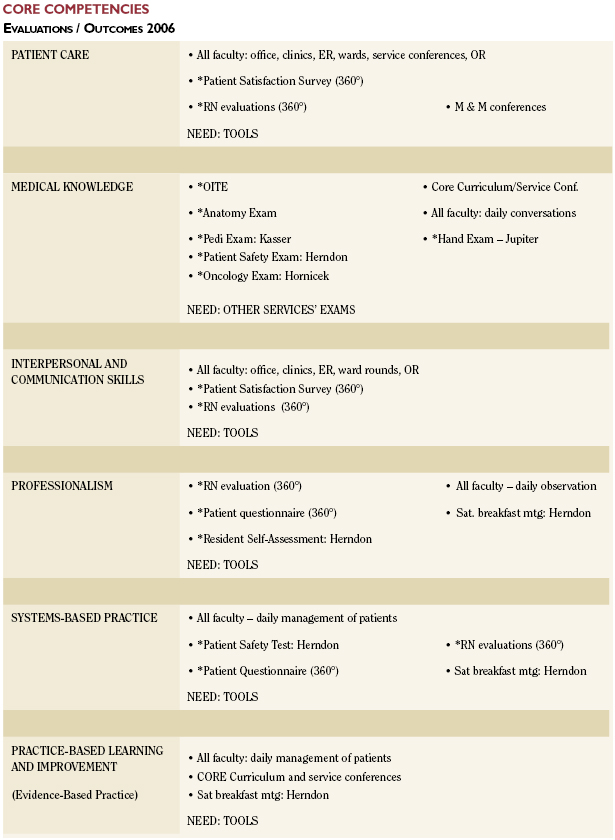
As you can see we need additional tools (as do other residency
programs) to measure the effectiveness of our teaching
success in these six categories. This is an evolving process and
in order to meet accreditation requirements each residency
program must demonstrate how they are progressing in the
implementation of tools to measure outcomes in each of the
six Core Competencies. A great deal of work is still required. All
residency programs are beginning to learn from each other and
we hope the ACGME will begin to provide accurate measurement
methods.
The Saturday breakfast program with the residency director
continues and remains successful. The following items have
been discussed at these breakfast meetings this academic year:

- Leadership issues
- Review of current revenues / expenses of Orthopaedic practices (Margin of Operations)
- New ICD- 9 / CPT codes
- Orthopaedic organizations – Alphabet Soup
- Review of HCORP graduates’ performance on ABOS exams
- Medicare payment changes
- Pay for Performance / Gainsharing Initiatives
- How to Start a Practice
- Financial Planning / Basics
- Initial Employment Contract - What to Look for and What to Avoid
This year, I have some additional time available, since I
no longer have the department chairman’s responsibilities and
I have voluntarily discontinued operating, (however, I still see
patients at the MGH and BWH and refer those patients needing
surgery to our colleagues). I have been reviewing our residents
and our residency program’s past performance regarding
work hours, success on Board examinations, success on the
Orthopaedic In-Training Examinations (OITE) and the surgical
experience of our residents before and after the 80 hour work
rule.
COMPLIANCE WITH WORK HOUR RULES
Our residents are burdened with a great deal of paperwork
today just as you are experiencing in your own practices.
Residents must now log their daily work hours electronically for
two months out of four during the year. The data is reported
directly to Partners Healthcare System and then to the ACGME
as well. The following is a brief analysis of our residents’ work
hours in the last two months:
- There were very few instances where the residents
worked more than 80 hours per week. We were in
compliance 98% of the time. There was only one
instance where the resident was on call more than
every third night and we were essentially 99% in
compliance.
- As we adjust to these new time demands and
constraints on our residents we are having difficulty
adjusting in three areas:
- The first is one day off in seven averaged
over four weeks. We had exceptions to this
in all five years of our residency program;
the majority being in the PGY 1 year. We
were in compliance only 76% of the time.
- The second is difficulty in compliance with
work > 24 hours. We had a significant
number of instances were residents worked
more than 24 hours straight. By far the
majority of these were in the PGY 1 years.
- A significant difficulty –which is a
problem for all surgical fields - is with the
requirement of at least 10 hours off between
shifts. A number of instances occurred where
residents did not have 10 hours off between
shifts. These exceptions occurred throughout
each year in the residency program. It has
been almost impossible to adjust resident
coverage when delays in the operating room
force elective surgery to be started in the
evening. Though we have a very large total
number of residents, there are only a few on
each service - spread too thin for residents
on other services to cover an elective case
starting early or late in the evening. There
are no “extra” residents - only those
residents on the service and, of course, they
are the ones taking care of the patients and
obviously want to participate in their
surgery. As a consequence residents often
only get five to eight hours off before
returning to work the next day.
The Executive Committee and faculty as well as the residents
are adjusting and adapting to these time constraints and
improvement has already been seen. I am optimistic that we
will be in full compliance before our next Residency Review
site visit.
EXPERIENCE OF BOARD EXAMS PART I AND II AND
ORTHOPAEDIC IN-TRAINING EXAM (OITE)
Over the last 16 years our residents have performed very
well on Part I and Part II of the American Board of Orthopaedic
Surgery examinations. However, only four times during this 16
years did 100% of our residents pass Part I on the first attempt
and on only five occasions pass Part II on the first attempt. Our
residents’ performances on the OITE have changed over the
last 31 years. Since 1989 there has been a steady improvement
in our percentile position (compared to other residencies) in
the examination. Residents now routinely score in the upper
two deciles. However, on careful analysis of each specialty,
reviewing each class and graduating classes, improvements
are needed. For example, in-training exam scores increased
in Pediatrics, Foot & Ankle, Sports and Shoulder during this
period of time, but no significant change occurred in Trauma
and Medical Issues. Surprisingly, there has been a slight fall in
the overall performance of our residents on Hip/Knee, Spine,
Hand, Orthopaedic Disease, Rehabilitation and Basic Science.
In view of this data, the Executive Committee and I are having
discussions with the faculty and the residents on how we can
improve. I have recommended to the Executive Committee and
the faculty that an individual on each specialty division take the
in-training examination yearly to ensure that our educational
program is in sync with what residents are expected to know
as determined by other national leaders. Each specialty division
chief will also be given his/her specialty data, including scores
on the ABOS exams and OITE exams. They will be able to use
the information to modify and change their teaching conferences
and Core Curriculum programs.
SURGICAL EXPERIENCE
I am monitoring the surgical experience of our residents,
in terms of volume and distribution of surgical cases and their
operating room experience as surgeon or assistant. There’s
no doubt that residents have little independence today compared
with 10 years ago because of the Medicare and ACGME
regulations - supervision is mandatory. It is very important
that without an extra six months of training as a chief resident
that our program meet the needs of our residents in terms
of providing them with the clinical and scientific educational
material, conferences, patient diversity and surgical experiences
that will allow them to be independent practitioners when they
graduate. Faculty will have to continue to meet challenges (as
do other faculties) on how to improve the surgical experience
of residents and most importantly how to measure residents’
performances regarding the six Core Competencies.
I have analyzed the surgical case volume of our graduating
residents comparing the graduates in 1999 to the graduates
in 2004. In 1999 we had no 80-hour work-week rule limitations.
The 80-hour work rules when into effect on July 1, 2003
and, although the 2004 graduates were not completely under
the new guidelines, they did function for one year with the
work hour’s restrictions. In addition we have made many
changes in the program such as Grand Rounds and the Core
Curriculum occupying five hours every Wednesday morning.
Conference schedules have increased because of the increased
number of specialty services and the residents are expected to
see outpatients at least one half if not one full day in clinics or
offices. With these changes and the work hour restrictions we
have seen a 27% increase in the volume of surgery recorded
by our residents in 2004 versus 1999. When comparing our
residents’ surgical experience to the mean surgical experience
of all residents in the United States (according to the Residents
Review Committee in 1999) we were 17% lower in terms of
total number of surgical cases. In 2004 with our significant
increase in surgical volume we were only 10% lower than the
mean national average. This is well within range of appropriate
surgical experience for residents; interestingly there was
also a significant increase in the average number of cases done
nationally in 2004 compared to 1999.
In conclusion there are some issues that I think are important
for the future of our orthopaedic residency program:
- Accurate and effective tools are needed to measure
the outcomes of our education and training program
in the six core competencies for all residents.
- Careful documentation of the residents’ surgical
cases, especially regarding whether they performed a
major portion of a case or were merely assistants.
It is important because program directors are
increasingly being asked to verify that the resident
is adequately trained to do procedures that are
often itemized in documents sent to the program
director. Obviously, with the public and payers
demanding increasing transparency of health care
regarding errors, quality, costs, and other factors,
so also will be the transparency of residents’
performance, training and experience. There appears
to be a general movement toward having the
program directors determine the competency of a
graduating resident regarding certain surgical
procedures.
- We will see increased use of simulation as a surgical
educational and assessment tool.
- Work hours limitations will definitely continue to
be enforced and we will be required to adhere to
them. Today it is law only in the State of New York,
but currently Congress is considering legislation to
make the work hour limitations law throughout
the United States. More importantly there are studies
that demonstrate an increased error rate when
ordering medications if someone has worked for
a straight sixteen hours. I think that we may see
a further reduction in the actual number of hours
residents are allowed to work each day in the future.
- Teaching goals and objectives are necessary as
well as a curriculum for each of the specialties’
fellowships similar to the residency program. These
requirements are increasingly being stressed by the
Residency Review Committee and the ACGME.
Residents are considered more as students and
less as providers of care by accreditation bodies.
However, Medicare continues to consider the
residents as service providers and, of course, pay
their salaries through Part A dollars for their
services. There may be movements that Medicare
to pay only for patient care provided by the residents
and not for any educational conferences or time
away from patient care for various reasons.
- With the increasing number of faculty at each
hospital and clinical care growth expected to
continue there will not be enough residents to
cover every attending and for every surgical case.
There will have to be future discussions about
service and education, teachers and non-teachers -
all very difficult issues.
- The very important and yet poorly understood and
poorly defined relationships of the residents with
fellows, with physicians’ assistants and with nurse
clinicians. There is some movement toward having
fellowship programs overseen by the residency
program director who is becoming the de facto
education officer of a department.
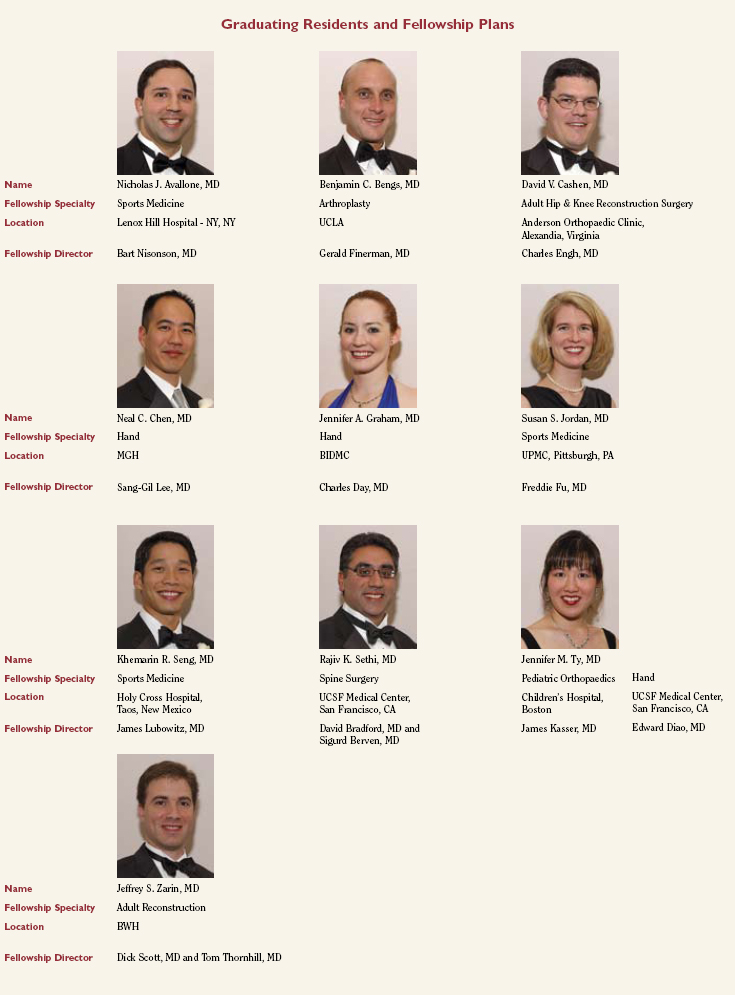
Awards
Two of our residents, John Kwon and Nick Avallone were nominated by the Harvard Medical School Class of 2006 for their
excellence in teaching. Congratulations to both John and Nick for receiving these outstanding recognitions by Harvard Medical
students.
Additional awards were received by: Andy Jawa and Nick Avallone. Andy received the Best paper at the OTA and re-presented
at AAOS on Trauma Specialty Day. The title of the paper was “Distal third extra-articular humeral shaft fractures: treatment with
bracing v. plating”. Nick was elected to AOA as an alumnus from UMDNJ - Robert Wood Johnson Medical School. The description of
the award is as follows: “This honor is in recognition of your demonstrated commitment to scholarly excellence, continued achievement
and excellence in medical education.” Also, Nick received a Partners-in-Excellence Award in December 2005 for service at
BWH during his time as Administrative Chief Resident.
The Barrett Family Research Awards were won by Dr. Susan Jordan for Basic Science and Dr. Nicolas Avallone for Clinical
Research. The Marmor Award for the overall best OITE average score was awarded to Dr. Benjamin Bengs.




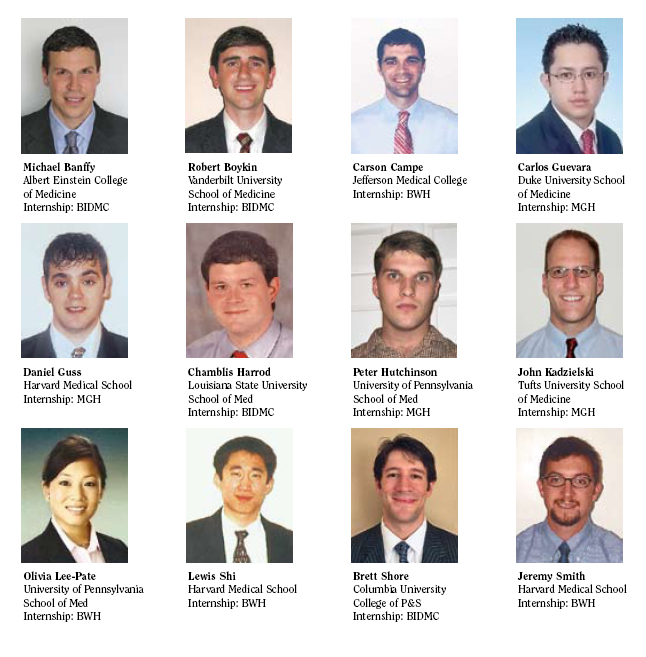
The Combined Orthopaedic Residency Program
PGY-2 Orthopaedic Residents
2006 - 2007
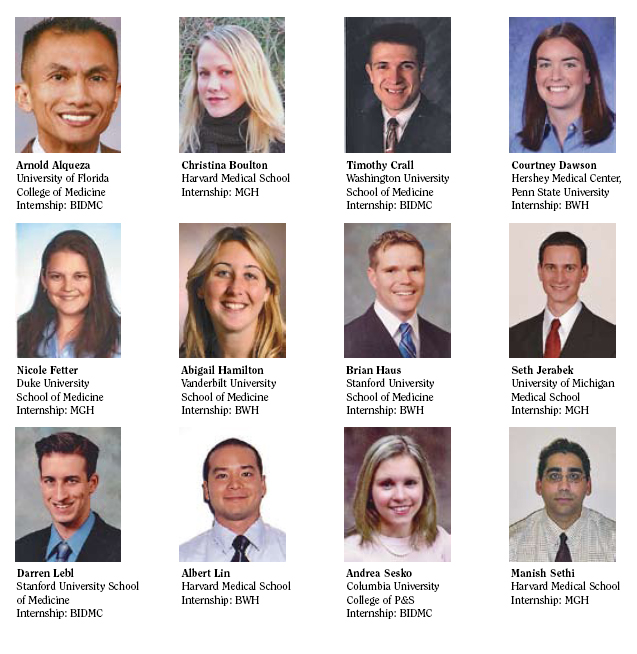
The Harvard Combined Orthopaedic Residency Program
Orthopaedic PGY 1 residents
Starting June 19, 2006
|

