Comparing Elbow Pathophysiology in Throwers Choosing Ligament Reconstruction to Those Who Do Not
Layla A. Haidar, BSA, Joost T.P. Kortlever, MD, David Ring, MD, PhD
The authors report no conflict of interest related to this work.
©2020 by The Orthopaedic Journal at Harvard Medical School
BACKGROUND Most professional baseball pitchers have pathological changes in their throwing elbow. This is detectable on imaging examination, surgery, and post-mortem. It is not clear when these changes in the elbow benefit from surgery to reconstruct the ulnar collateral ligament (UCL) with a tendon graft. We systematically reviewed published data on throwing athletes to address the following questions:
- Do throwers that decide to have a ligament reconstruction have worse objective signs of pathology than those that do not?
- Does pathology progress in throwing athletes?
METHODS We searched on PubMed for scholarly and original articles discussing UCL injury routine screening, use of magnetic resonance imaging (MRI), radiographs, or physical examination of throwers, and studies stating differences in why athletes chose to have UCL reconstruction. We looked for studies that met the following inclusion criteria: studies of UCL insufficiency of the elbow in throwing athletes and information about radiological appearance, motion, or laxity of the elbow, and original data.
RESULTS Throwers having ligament reconstruction had less pathology than those having screening or nonoperative treatment. Throwers that had ligament reconstruction at age 21 to 23 had worse pathology than throwers aged 17 to 21.
CONCLUSION Our observations suggest that professional baseball pitchers are generally adaptive to the inevitable elbow pathology. The decision of throwers to seek care and accept offers of UCL reconstruction does not seem related to severity of pathology, which suggests accommodation can be an effective strategy.
LEVEL OF EVIDENCE Level III Systematic review of diagnostic studies
KEYWORDS Thrower’s elbow, ulnar collateral ligament, reconstruction, pathophysiology, imaging
The ulnar collateral ligament (UCL) of the elbow can become attenuated in athletes that throw an object overhead frequently and with great force. The UCL of the elbow represents one of the most prevalent problems in the throwing arm amongst baseball players, pitchers in particular.7 Attenuation of the ligament is associated with a specific pattern of osteoarthritis (valgus impaction overload). Reconstruction of the UCL using a tendon graft was popularized after pitcher Tommy John was able to continue pitching professionally after having the surgery in 1974. It has since gained an unwarranted reputation for improving the performance of pitchers who undergo the procedure.20 However, it is important to say that this procedure has provided a relatively successful solution to a once career-ending injury.
Most professional baseball pitchers have pathological changes in their throwing elbow.22 It is not clear when these changes in the elbow benefit from surgery to reconstruct the ulnar collateral ligament with a tendon graft. Both the offer of surgery and the decision to pursue surgery seem subjective and preference-sensitive.
We systematically reviewed published data on throwing athletes to address the following questions:
- Do throwers who undergo a UCL have reconstruction have worse objective signs of pathology?
- Does elbow pathology progress over time among throwing athletes?
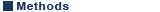
Study design
We report our results according to the PRISMA Statement. Between March 26th-April 5th, 2018, we searched on PubMed for scholarly and original studies on UCL injury routine screening, use of MRI’s, radiographs, or physical examination of throwers, and studies stating differences in why athletes chose to have UCL reconstruction using combinations of the following keywords: "throwing", "throw", "pitcher", "athlete", "elbow", “ulnar collateral ligament", "UCL", "pathology", and "pathophysiology" in title and abstract. Our literature review encompassed the years of 1994-2018. Two reviewers (LH and JK) independently screened titles and abstracts and subsequently full texts using predefined criteria. We looked for studies that met the following inclusion criteria: studies of UCL insufficiency of the elbow in throwing athletes and information about radiological appearance, motion, or laxity of the elbow, and original data. We excluded case reports, letters to editors, meeting abstracts, reviews, and meta-analyses. After our initial screening, a total of 39 articles remained (Figure 1). Thirteen articles were excluded after reading the abstract and 5 articles were excluded after full text review because of insufficient or irrelevant data that did not answer our study questions, leaving 21 studies for data retrieval (Table 1).
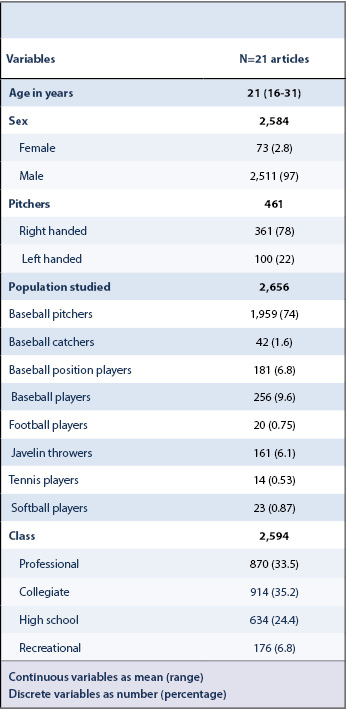
For each of these 21 studies we recorded the population studied (baseball pitchers, catchers, or position players, football players, javelin throwers, tennis players, softball players), study type, year of study, sports level (professional, collegiate, high school, recreational, or a throwing athlete in general), age in years, sex, and whether they had ligament reconstruction, were on the disabled list, were right or left handed, had radiographic abnormalities (medial joint space widening during valgus stress radiographs, presence of olecranon osteophytes, calcification within the UCL substance, laxity with valgus stress testing, or radiologist diagnosed partial or complete tears on MRI), moving elbow stress test negative or positive, and pain or no pain with the valgus stress test.
We reported continuous variables using mean and range and discrete data as number and percentages. Differences between outcomes were assessed using Fisher’s exact tests. We considered P <0.05 significant.
More than 90% of the subjects were baseball players with varying levels of experience, 80% pitchers (Table 2). One-hundred twenty-seven throwers were evaluated as part of a routine pre-season screening process, 155 were being treated nonoperatively, and 2,238 had UCL reconstruction with a tendon graft.
Throwers having ligament reconstruction had less elbow pathology than those having screening or nonoperative treatment (Table 3). There was a lower percentage with medial joint space widening under valgus stress (N=1,015, 47% vs N=173, 100%; P <0.001), olecranon osteophytes (N=208, 13% vs N=15, 28%; P=0.004), and calcification within the UCL substance (N=182, 12% vs N=38, 30%; P <0.001).
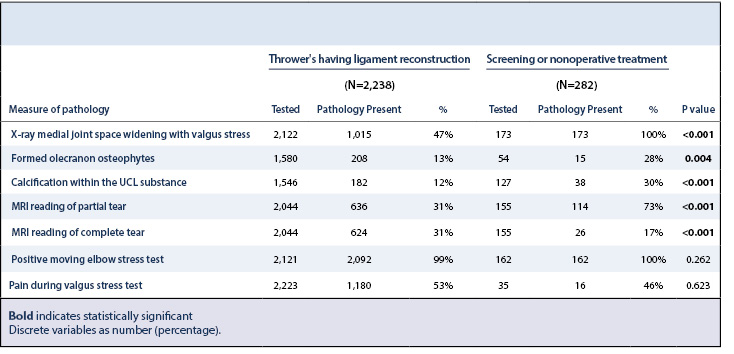
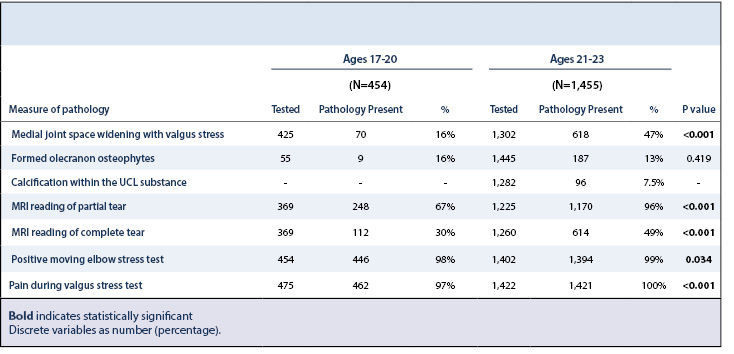
Throwers that had ligament reconstruction in the 21-23 years of age group had worse pathology – specifically more throwers had increased medial joint space (N=618, 47% vs N=70, 16%; P <0.001), positive moving elbow stress test (N=1,394, 99% vs N=446, 98%; P=0.034), and pain during the valgus stress test (N=1,421, 100% vs N=462, 97%; P <0.001) – compared to throwers who had ligament reconstruction in the 17-20 years of age groups (Table 4).
Professional baseball pitchers with an attenuated UCL may consider reconstruction with tendon graft in order to continue throwing. Given that the decision to pursue surgery is relatively imprecise and subjective, we sought objective measures of pathology such as radiological (MRI, radiograph) and physical examination data of throwing athletes, comparing those being screened as part of a routine physical examination process or being treated nonoperatively with those requesting ligament reconstruction.
Our study has limitations. First, we only identified 21 studies based on our inclusion criteria. We only used PubMed for our search. We found articles specific to UCL injuries, and baseball players which was the focus of our paper. It is possible searching in other databases would yield more articles. This could influence results by not looking at all data appropriately. However, we also went through the reference lists to check for additional articles. Second, it was not possible to isolate baseball pitchers from other athletes, as was our intention initially. It might be that different ways of throwing contribute differently to (the location of) pathophysiology. Third, as is usual the case when comparing multiple studies, we had different and varying data from each study. Not all data was assessed or mentioned in each study and different methods were used, which hindered comparisons. This could affect the accuracy of our data. Fourth, there were large sample size differences between non-operative, and operative subjects which could lead to a source of bias.
Among 21 studies that reported pathology data we found that throwers who had ligament reconstruction had significantly less objective pathology than throwers that were screened or treated nonoperatively. Medial joint space widening with the valgus stress test, olecranon osteophytes, and calcification within the UCL substance seem as common or more common in effective throwers as they are in those that choose reconstruction. This suggests that decisions to seek care and a decision for surgery may be based largely on discomfort when throwing. This includes both surgeon offer of surgery and patient decision to proceed. Using subjective criteria to determine the appropriateness of UCL reconstruction risks unhelpful surgery and may hinder attention to more effective interventions that help throwers adapt like their counterparts with similar objective pathophysiology. It is possible that the subjective basis of most ligament reconstructions is contributing to a notable rise in the rate of ligament reconstructions.6 Given that so many professional pitchers perform well in spite of pathology, the role of UCL reconstruction remains incompletely defined.
The observation that throwers aged 21-23 years of age have greater pathology than throwers between the ages of 17-20 years of age, is consistent with the concept that baseball pitchers gradually and perhaps inevitably develop changes in their elbow if they continue to throw at a high level for several years. Our findings are consistent with a recent study of young professional baseball pitchers aged 17-21 years, in whom stress ultrasound (SUS) of the elbow was performed to assess changes in the anterior band of the UCL, that found UCL thickness increases as the years of professional pitching experience increases.2
While more study is needed to be certain, these results suggest that something other than measurable pathology may be inducing throwers to seek care and accept offers of UCL reconstruction. These less studied subjective (or less measured) factors may be more prone to lower reliability and accuracy and may be more subject to issues of appropriateness. These subjective factors may also affect outcomes. Such as, if a thrower who is less adaptive to elbow pathology is more likely to choose surgery, the ability to return to the prior level of play might benefit from efforts to optimize adaptiveness, for instance with cognitive behavioral therapy and its variations. Our observations suggest that professional baseball pitchers are generally adaptive to the inevitable elbow pathology. A better understanding of the factors supporting this adaptiveness could be of benefit.