Functional Outcomes and Complications of Radial Head Fractures Treated with Screw Fixation
Jonathan Lans, MD, PhD, Nicolas Galli, MD, Daniel Mattera, MD, Alberto Fernandez Dell’Oca, MD, Neal C. Chen, MD, Jesse B. Jupiter, MD
The authors report no conflict of interest related to this work.
©2020 by The Orthopaedic Journal at Harvard Medical School
BACKGROUND Open reduction and screw fixation or radial head arthroplasty can both be performed to treat comminuted radial head fractures.
OBJECTIVE In this study, we evaluated the functional and patient reported outcomes of complex radial head fractures treated by bouquet screw fixation.
METHODS A retrospective analysis of all patients with a complex radial head fracture treated with bouquet screw fixation from February 2008 to April 2016 at a single institution was performed. Eighteen patients were included with a median follow-up of 42 weeks. Complications and range of motion at final follow up were collected for all patients. Postoperative Quick Disabilities of the Arm, Shoulder and Hand (DASH) scores were completed by 16 patients.
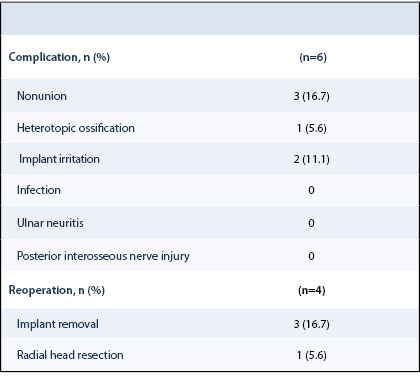
RESULTS The median QuickDASH score was 4.5 (IQR: 4.5-12.5). There were six complications including nonunion (3/18), implant irritation (2/18) and heterotopic ossification (1/18). There were significantly more nonunions in patients with more than two fracture fragments (P=0.043). Four patients underwent reoperation: three implant removals and one late radial head resection.
CONCLUSION Bouquet screw fixation may be problematic if greater than two radial head fragments are present in complex radial head fractures.
LEVEL OF EVIDENCE Level IV Therapeutic Study
KEYWORDS Radial head fracture, open reduction internal fixation, outcomes, complications
Radial head fractures account for one-third of all elbow fractures and often result from a fall onto the outstretched arm in pronation. When other injuries are present, the radial head fracture may be unstable.1 Reconstruction of the lateral column maintains the normal axis of the elbow and reduces the risk of degenerative arthritis in both the elbow and wrist joints.
Surgery is recommended when there is impaired forearm motion, >2 mm fracture displacement, or if >1/3 of the radial head diameter is fractured.2-6 Open reduction and internal fixation (ORIF) should be considered for comminuted fractures of the proximal radius with excellent long-term results.7,8,17,19-16 However, overly aggressive use of ORIF places the patient at risk for failure (pseudoarthrosis, mechanical failure, osteonecrosis). In the face of non-reconstructable radial head fractures, the alternatives to ORIF include radial head excision or arthroplasty (RHA). RHA produces excellent results in 85% of cases but may have higher complication rates.3,18,27-32,19,26 Radial head excision in complex radial head fractures results in inferior outcomes compared to radial head ORIF, and this may be related to osteoarthritic changes following excision.24,33
The aim of this study was to evaluate the functional and patient reported outcomes, as well as the complications, of complex radial head fractures treated with screw fixation in a setting where radial head arthroplasty was not available. We hypothesized that screw fixation of radial head fractures can result in acceptable outcomes.
After ethics committee approval, we performed a retrospective analysis of all patients with a radial head fracture treated with screw fixation at an urban level IV trauma center in Uruguay from February 2008 to April 2016. Patients above the age of 18 years were included. Indications for operative treatment were partial articular radial head fractures with displacement >2mm, displaced radial head fractures with greater than one fragment, or restricted supination or pronation. Five patients with isolated radial head fractures were excluded. Complex radial head fractures were defined as fractures with accompanying injuries of the elbow. All patients underwent a standard preoperative computed tomography (CT) scan to determine fracture characteristics. All preoperative and postoperative radiographs are accessible through the ICUC iPad application Database (http://www.icuc.net/), along with intraoperative photographs, fluoroscopy images, and photographs of the final range of motion. The in-application cases can be found in Appendix 1.
Study Population
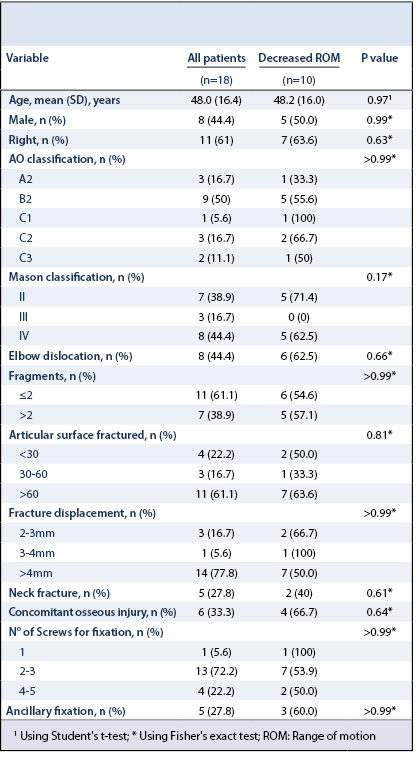
Eighteen patients were included. There were 8 males and 10 females with an average age of 48.0±16.4 years (range: 22-71) and median radiographic follow-up of 42 weeks (range: 10-125) (Table 1). Using the modified Mason-Johnston classification, there were 7 Mason II fractures, 3 Mason III fractures, and 8 Mason IV fractures.34,35 Using the Association for the Study of Internal Fixation Comprehensive Classification of Fractures, 3 fractures were classified as A2, 9 were B2, 1 was C1, 3 were C2 and 2 were C3.36 All patients had an associated collateral ligament injury and 6 patients had an associated fracture of the ulna, including 3 olecranon fractures, 1 coronoid fracture, 1 diaphyseal and 1 metaphyseal fracture. Eight patients had an elbow dislocation, where 2 had a terrible triad injury of the elbow. There were 2 patients with Monteggia fractures. No patients had an Essex-Lopresti lesion.
Operative Treatment
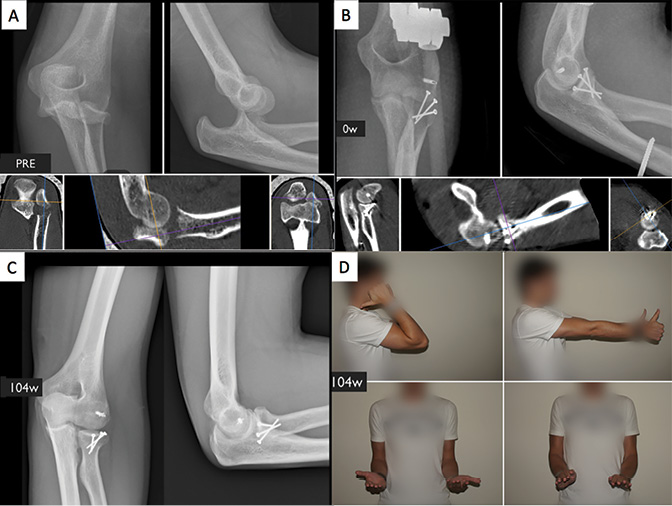
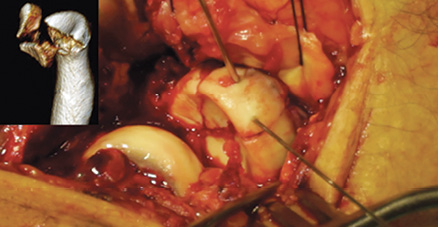
All patients underwent surgery within three days after injury by a single traumatologist. Radial head arthroplasty was not available at the institution because of financial constraints, so the routine practice is radial head fixation. When there was a solitary radial head fracture, a lateral approach was used. The radial head was approached through the Kocher interval (between the extensor carpi ulnaris and anconeus muscles) in 11 patients, through the Kaplan approach (between the extensor digitorum communis and extensor carpi radialis brevis muscles) in 6 patients, and a posterior approach to the elbow in one patient.37,38 To achieve complete visualization of the radial head, the muscles attached to the lateral supracondylar ridge were released. In the presence of lateral collateral ligament injury, this was reattached to the lateral humeral epicondyle using a suture anchor (Mini Quickanchor, DePuy Synthes, West Chester, Pennsylvania, USA). Cortical positioning screws sized 1.5mm to 2.0mm ranging from 18 mm to 34 mm in length (DePuy Synthes, West Chester, Pennsylvania, USA) were used, and the number of screws was determined intraoperatively. The screws were placed transversely or obliquely in the area of safety as bicortical positioning screws without compression.39 Most patients (13 of 18) were treated with 2-3 screws, followed by 4-5 screws (4 of 18), and one patient was treated with a single screw (Figure 1 and Figure 2). Bone grafting was not performed in any patient. Either a posterior approach, a Kocher approach through the posterior incision, or a combined posterior and lateral approach was used in the presence of a concomitant ulna fracture. Four patients had fixation of the ulna using a Locking Compression Plate (LCP, DePuy Synthes, West Chester, Pennsylvania, USA) and one patient had an olecranon fracture treated with tension band wiring. Eight patients had an accompanying elbow dislocation, and all eight were treated with a static external fixator for three weeks. Postoperatively, the patients who did not have a fixator were immobilized for 10-14 days in an upper arm cast in 90° flexion and neutral supination/pronation followed by gradual, patient-directed mobilization. Active motion began after 5-6 weeks.
Evaluation
All patients were clinically assessed by the treating physician at final follow-up, and the range of motion (flexion, extension, supination and pronation) was documented using photographs. Range of motion was calculated as a percentage of the uninjured elbow. A satisfactory outcome was defined as a range of motion of at least 90% of the uninjured elbow. As a patient reported outcome measure, we used the Quick Disabilities of the Arm, Shoulder and Hand (qDASH) score (Spanish version), where a score of 12.7 is normal for a working population.40 The senior author and an orthopaedic resident performed the final radiographic evaluation regarding fracture healing. Reoperation, nonunion, infection, implant irritation, nerve injury, or heterotopic ossification were considered complications. The presence of ligament injury was based on the intraoperative findings.
Statistical Analysis
To evaluate factors influencing range of motion, we used the Fisher’s exact test for nominal variables and the Student’s t-test for parametric continuous variables. The Fisher’s exact test was also used to test if fracture characteristics influenced the incidence of complications and reoperations. A Mann-Whitney U test was used to assess if fracture characteristics, complications, or decreased range of motion influenced the qDASH score. A significance level was set at 0.05 for all tests.
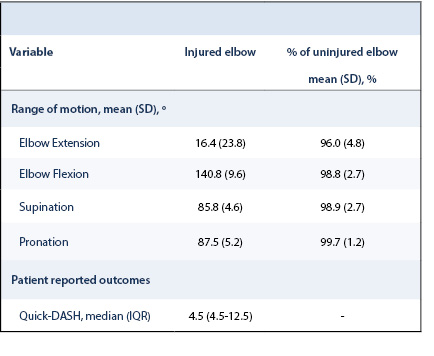
The average elbow extension was 16.4°±23.8, flexion was 140.8°±9.6, supination was 85.8°±4.6, and pronation was 87.5°±5.2. Compared to the uninjured elbow, the injured elbow had 98.8±2.7% flexion, 96.0±4.8% extension, 98.9±2.7% supination and 99.7±1.2% pronation (Table 2). All patients achieved a satisfactory range of motion of >90% when compared to the uninjured elbow. In eight (44.4%) patients, there was no difference in range of motion between the injured and uninjured elbow.
We were able to contact 16 patients to complete the qDASH at least 11 months postoperatively, of which six had a complication. The median postoperative qDASH score was 4.5 (range: 0-61.4). The median qDASH score for patients with reduced range of motion was 18.4 (range: 0-61.4) compared to 4.6 (0-13.6) in those without reduced motion (P=0.62). Patients with complications had a median qDASH of 9.1 (range: 4.6-61.4) and the qDASH was 4.6 (range: 0-52.3) in those without complications (P=0.17).
There were six patients with complications (case 4, 8, 16, 18, 21, 22) including four who underwent reoperation (Table 3 and Table 4). Complications occurred in 4 of the 7 fractures with more than two fragments compared to 2 of the 11 fractures with two or less fragments (P=0.14). Nonunion only occurred in the fractures with more than two fragments (3 of 7) and did not occur in the fractures with one or two fragments (0 of 11) (P=0.043) (Table 5).
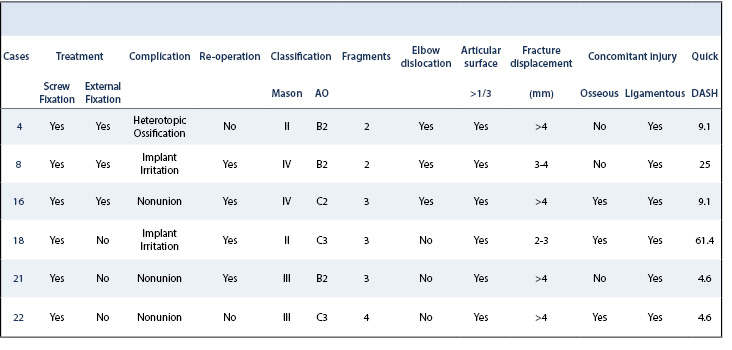
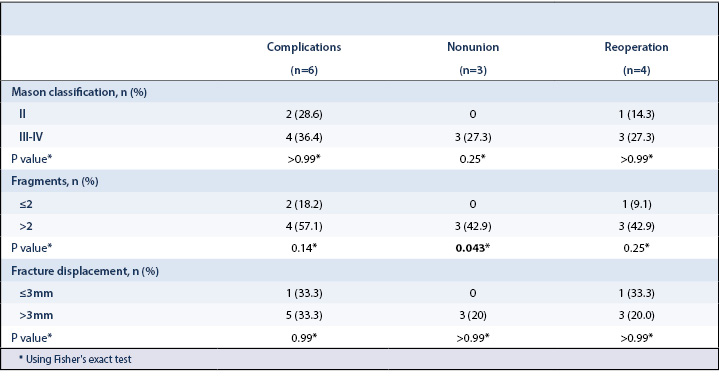
The most common complication was nonunion (case 16, 21, 22), followed by implant irritation (case 8 and 18) and heterotopic ossification (case 4). The respective qDASH scores are reported in Table 4. Two patients with nonunion had a reoperation. One (case 16) underwent radial head resection because of an unstable nonunion while the other underwent implant removal because the radial head was found to be a stable, fibrous union intraoperatively after implant removal (case 21). The other patient with nonunion had no pain or functional impairment (case 22). Complete or partial implant removal was performed in two patients (case 8 and 18) because of implant irritation (Figure 3).

In this study, screw fixation of complex Mason II, III and IV fractures was a viable treatment option resulting in a median qDASH score of 4.5 with all patients obtaining a satisfactory range of motion. Despite these favorable outcomes, complications were frequent—occurring in 1 in 3 cases with roughly 1 in 5 cases undergoing reoperation. Nonunions were more common in fractures with more than two fragments. Our results are comparable to prior studies demonstrating an incidence of nonunion and reoperation ranging from 4% to 44%.3,7,16,21,22,24,26,28-32,8,41,9-15
In this study, patients with more than two fragments had a significantly higher incidence of nonunion, 43% versus 0%. Prior studies have reported a higher rate of complications in radial head fractures with these characteristics.22,23,29,30,32 A comparable study by Al-Burdeni et al. reported a qDASH of 14.1 and a complication rate of 78.9% in 19 patients with Mason III and Mason IV fractures of which 8 were treated with screw fixation.22 Similarly, Wu et al. described good outcomes and a lower reoperation rate (6.5%) in 31 Mason II, III and IV radial head fractures treated with headless compression screws.17
Ring et al. retrospectively evaluated 56 radial head fractures treated by ORIF and recommended that patients with more than 3 articular fragments (Mason III) should be treated with arthroplasty.32 Although our results again demonstrate that more complications occur when there are 3 or more fracture fragments, we do believe that screw fixation can be a good treatment option in these patients when used judiciously. Notably, in the study by Ring et al., 92% of the Mason II fractures were treated with screw fixation whereas 85% of the Mason III fractures were treated with plate fixation. A higher complication rate after plate fixation compared to screw fixation has been reported, and it is not clear to what degree this affected the results.21 Although the study has been influential, no definitive conclusion regarding screw fixation in Mason III fractures can be drawn.
The evidence regarding superiority between ORIF and arthroplasty in reconstructable Mason III or IV patients is inconclusive.21,23,24,29,30 To date, there is one randomized-controlled trial by Chen et al. in which unstable Mason III fractures were randomly assigned to be treated with ORIF (n=23, screws and plates) or arthroplasty (n=22).31 The authors reported a satisfactory outcome according to the Bromberg and Morrey score in 91% of the arthroplasty patients compared to 65.2% patients in the ORIF group. Also, they reported a significantly higher rate of complications in patients with ORIF (47.9%) than in those undergoing arthroplasty (13.6%). Additionally, Pogliacomi et al. described superior outcomes of arthroplasty in Mason IV fractures.42
Our outcomes using screw fixation were comparable to radial head arthroplasty. Marsh et al. described 55 patients treated with a radial head arthroplasty and a minimum follow up of 5 years achieving an average qDASH score of 14.43 However, there are questions about the long-term durability of radial head arthroplasty. Mid-term results have shown DASH scores ranging from 14-23 in patients treated with a press-fit radial head arthroplasty, but implant removal was performed in almost a quarter of the patients and a reoperation rate of 38.9% of was reported.19,44 In light of this developing data, preserving the native radial head may have long-term advantages.
We need to interpret these results with respect to the study’s strengths and limitations. First, the study reports the results of a single surgeon with many years of experience as a traumatologist. Therefore, these results may not be generalizable. In addition, examiners evaluating results and radiographs were not blinded and this was a single center study, which may both introduce bias. Secondly, the radiographic follow-up was short (median 42 weeks), so the development of osteoarthritis could not be evaluated. Patients may undergo further reoperations as follow-up increases; however, patient outcomes may also improve. Third, patients with elbow dislocations were treated with external fixation for 3 weeks, which has a separate influence on outcomes. Lastly, this was a small cohort consisting of only 18 patients, and injury patterns varied.
This study provides value by reporting the outcomes of homogeneously treated complex radial head fractures in a setting where radial head arthroplasty was not available. Most contemporary studies evaluating radial head ORIF are confounded because more complicated fractures are often treated with arthroplasty.
In conclusion, complex but reconstructable Mason II, III and IV radial head fractures can be treated with screw fixation with reasonable outcomes.17,19,44 Although complication rates are higher, there may be advantages to radial head preservation as it is less expensive than a radial head arthroplasty, and a radial head arthroplasty may still be performed as a salvage procedure. If it is possible to achieve good outcomes with radial head preservation, renewed interest in radial head fixation may be worthwhile.