New Patient Visit for Care of Idiopathic Trapeziometacarpal Osteoarthritis: Factors Associated with Injection and Radiographs
Janna S.E. Ottenhoff, MD, Anne-Britt E. Dekker, MD, David Ring, MD, PhD
The authors report no conflict of interest related to this work.
©2020 by The Orthopaedic Journal at Harvard Medical School
BACKGROUND Radiographs may have limited utility in the diagnosis and management of trapeziometacarpal osteoarthritis (TMC OA). In the two trials performed to date, intra-articular steroid injection does not relieve symptoms better than simulated steroid injection. The goal of this study was to assess the prevalence of, and factors associated with obtaining radiographs and performing intra-articular injection at new patients visits for idiopathic TMC OA.
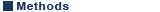
METHODS Two thousand nine hundred sixty-one eligible patients with TMC OA were identified in a national administrative claims database for commercially insured patients. We created two multivariable logistic regression models to identify independent factors associated with (1) radiograph and (2) injection at first visit.
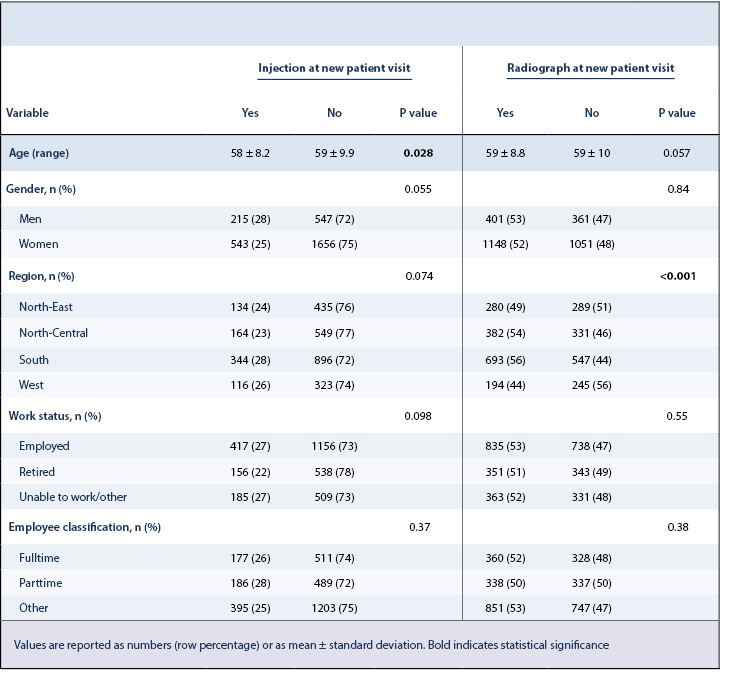
RESULTS Approximately half of the patients (1549 of 2961; 52%) had a radiograph during their first evaluation of TMC OA by a surgeon. In multivariable analysis, patients from the southern United States correlated with greater rates of radiographs obtained at first visit. Nearly one quarter of the patients (758 of 2961; 26%) had an injection during their first evaluation of TMC OA by a surgeon. In multivariable analysis, women were associated with a lower likelihood to receive an injection during a new patient visit.
CONCLUSION Our study showed a high prevalence of radiographs and intra-articular injections among patients with TMC OA coded as a new visit. The discordance between daily practice and current best evidence merits attention.
LEVEL OF EVIDENCE Level IV Cross-sectional Study
KEYWORDSOsteoarthritis, thumb, injections, intra-articular, radiography, outpatients
Trapeziometacarpal osteoarthritis (TMC OA) is an expected part of human ageing.1-3 Studies identify incidental, advanced, and well adapted TMC arthrosis as a common finding among people seeking care for other problems.1,2 The true prevalence of patients with TMC OA seeking specialty care is unknown but evidence suggests that most people adapt to their condition.1,2,4,5 With respect to knee OA, population based studies of people over 65 years of age demonstrate a high prevalence of osteoarthritis but most people seem to adapt to their condition, even with advanced disease. For instance, less than half of the patients with the most advanced radiographic findings of knee OA qualified as having symptomatic arthritis.6 Based on this, and the high prevalence of radiographic TMC OA found in prior studies, it seems reasonable to infer that population-based studies of TMC OA would have similar findings.1 Studies of people with crepitation of the TMC joint (“incidental TMC OA”) who are being seen by a hand specialist for other medical reasons suggest that—as with knee arthritis—TMC OA may be generally well-accommodated.3
Radiographs seem to have limited value in the management of TMC OA. The high prevalence of TMC OA and the characteristic symptoms and signs make diagnosis reliable and accurate without radiographs.1,2 Additionally, radiographs are not helpful in the treatment decision-making process, given the limited correspondence of radiographic severity of TMC OA with pain intensity and magnitude of physical limitations.4,7 Thumbs with crepitation during axial pressure and circumduction of the TMC joint (the so-called grind test) have advanced arthrosis.8
Intra-articular injections—with either corticosteroids or hyaluronic acid—provide brief palliation at best and cannot modify the natural history of the disease.9-15 It is not clear that therapeutic injections outperform placebo injection.9-15 A level I randomized controlled trial comparing hylan, steroid and placebo injections for CMC1 OA did not show significant differences in outcome.16 The only other study of corticosteroid injection compared to simulated steroid injection (saline) also showed no differences.10 A prior database study among three affiliated urban hospitals documented wide (51-fold) surgeon-to-surgeon variation in the rate of injections for TMC OA.17 There is evidence that treatment offerings are influenced by surgeon values and surgeon personality.18-21 Ideally, variation in treatments for TMC OA is based on patient values and preferences, not on surgeon bias.
This study assessed the prevalence of, and factors associated with obtaining radiographs and performing intra-articular injections for idiopathic TMC OA at new patient visits.
Study Design
This study was exempt from Institutional Review Board approval since no identifiable health information was reviewed. We used an administrative claims database for commercially insured patients (Truven Health Analytics Marketscan®) from October to December 2015. Inclusion criteria were patients with a diagnosis (International Classification of Diseases, Tenth Revision (ICD-10) code) of TMC OA and Current Procedural Terminology (CPT) codes for a new outpatient office visit (99201-99205) (Appendix 1). We used CPT codes on the same date to identify injection of small/intermediate joint (20600, 20604, 20605), and radiograph of the hand/finger (73120, 73130, 73140) (Appendix 1).
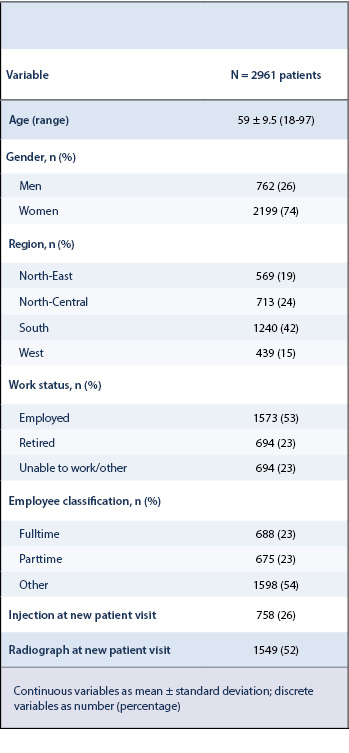
We included 3077 patients aged 18 years or older diagnosed with TMC OA at a new outpatient visit with a surgeon between October and December 2015. The following categories were analyzed for each patient: age, gender, geographic region (within the United States), work status, and employment classification. We excluded duplicate diagnoses claims (N = 36), claims with unknown region (N = 6), and those with a diagnosis of secondary (N = 29), or post-traumatic (N = 45) TMC OA.
Study Population
Two thousand nine hundred sixty-one patients were eligible, including 2199 (74%) women (Table 1).
Stastical Analysis
Continuous variables are reported as mean with standard deviations (SD) and discrete variables as number with percentage. We used Chi-squared test to compare categorical and dichotomous variables, and Student’s t-test for continuous and dichotomous variables.
We created two multivariable logistic regression models to identify independent factors associated with (1) radiograph and (2) injection performed at first visit. We included all factors with P<0.10 on bivariate analysis in the final models. C-statistic is a measure of goodness of fit in logistic regression model with scores between 0.50 and 1.00. Higher scores indicate a better fit. Semi-partial R2 expresses the specific variability of a given independent variable in the model.
Radiograph at new patient visit
Just over half of the patients (1549 of 2961; 52%) had a radiograph during a new patient evaluation of TMC OA. In bivariate analysis, there was a significant difference of radiograph rates between regions (P< 0.001) (Table 2). Accounting for potential interaction of variables using multivariable analysis, patients from the Southern United States (Odds Ratio [OR] = 1.3, 95% Confidence Interval [95% CI] = 1.1 to 1.6, semi-partial R2 = 0.0036, P = 0.009) correlated with greater rates of radiographs obtained at a new patient visit (Table 3).
Radiographs and injections have arguably limited utility in the diagnosis and management of TMC OA.12,17,19,22-25 Wide surgeon-to-surgeon variation in the use of radiographs and injections was observed in a prior study of six surgeons.17 This study assessed the prevalence of, and factors associated with radiographs and intra-articular injection for idiopathic TMC OA at new patient visits using a large national claims database.
We acknowledge several limitations to our study. We relied on a claims database and could not determine the completeness or accuracy of the data. Database studies cannot address effectiveness or satisfaction. We cannot tell from the database what substance was injected, but it seems safe to assume that the vast majority were corticosteroid injections. The database did not have surgeon level data, so we could only test variation among the four recorded geographic divisions of the United States.
The observation that more than half of the patients (52%) had a radiograph during a new patient evaluation of TMC OA suggests that radiographs are obtained routinely in many practices. The percentage of patients with TMC arthrosis that have a radiograph of the hand at some point in their care is likely larger, given that we could not account for patients that had a radiograph prior to this visit (from their primary care doctor or another specialist) or at subsequent visits. It is notable that in such a large percentage of patients with TMC OA radiographs are obtained when it offers few potential benefits and incurs costs and some potential harms. On the one hand, symptoms and physical examination are sufficient for accurate diagnosis of TMC OA in such a high-prevalence setting (after the age of 50 nearly half of all humans have some TMC OA).1,2,4,26,27 On the other hand, radiographic severity does not correlate well with symptoms and physical limitations and therefore will not be particularly helpful in the treatment decision-making process.27,28 In a recent review published in the New England Journal of Medicine the authors explain how symptom intensity and the magnitude of self-reported activity limitations are influenced by the way a (medical) condition is described and framed.29 In other words, the meaning or context attributed to the symptoms, often referred to placebo and nocebo effects. For example, mentioning potential side effects of an intervention can result in a more unpleasant experience.29,30 With respect to people presenting with symptoms of TMC OA, without radiographs, it might be easier to consider themselves as having age-appropriate changes in the their thumb instead of suffering from thumb OA.1,17,26 An adaptive interpretation of symptoms and limitations from thumb arthritis can potentially help to diminish pain intensity and improve self-reported activity level through psychosocial effects that are increasingly well understood.3,28,31,32 We suggest to increase the attention towards social and mental health in surgeon offices and offer psychosocial interventions to patients with TMC OA seeking care. In our opinion, patients with pain at the base of the thumb might consider asking their doctor about the potential benefits and potential harms associated with radiographs and whether they are worth the cost.
The finding that one in four patients with TMC OA received an injection during their new visit merits attention given that injections are palliative at best and may not outperform placebo injections.10,12,15,33 Keeping in mind that some patients likely received an injection prior to this visit (from their primary care doctor or another specialist) or at subsequent visits, the percentage of patients with TMC arthrosis that receive an injection at some point in their care is likely to exceed 26%. It is notable that such a large percentage of patients with TMC OA receive an injection when the evidence suggests no benefit.10,16 It is also important to consider the potential harms of injection. Corticosteroid injections can be detrimental to articular cartilage and are associated with skin-related adverse events.9,12-15 We wonder if people would choose an injection if they were more aware of these aspects and if this would lead to less surgeon-to-surgeon variation in injection rates. It is important that clinicians help patients consider what matters most to them to ensure that decisions are based on patient values rather than on misconceptions and not on surgeon bias. Common misconceptions to be vigilant for include the belief that the injection can cure the problem or is in some way necessary. Given the evidence that injections are over-utilized relative to the available evidence, combined with the knowledge that injections have potential physical and psychosocial harm, injection for TMC OA might be considered for inclusion on the Choosing Wisely campaign.34 We recommend that physicians inform their patients to seek unbiased information – e.g. by reviewing a decision aid35 – and be prepared with questions if their doctor offers an injection for TMC OA.
Our study showed a high prevalence of radiographs obtained and intra-articular injections given at new visits among patients seen for TMC OA. Given the weak correspondence of radiographic severity and TMC OA symptom intensity, and the knowledge that steroid injections do not provide greater relief than placebo injections, these might represent areas for cost savings. Besides that, it’s important to consider the strong influence of cognitive biases regarding pain (e.g. catastrophic thinking and fear of painful movement) and the influence of context effects (e.g. placebo and nocebo) on patient symptom severity and the magnitude of self-reported activity limitations. We recommend that patients presenting to a hand surgeon with base of thumb pain ask their surgeon whether and how diagnostic tests, like radiographs, are helpful and to which degree injections or other recommended interventions fit their goals and values.