A Novel Technique for Fixation of a Medial Femoral Condyle Fracture using a Calcaneal Plate
Eric C. Loesch, BS, Ankur B. Bamne, MBBS, MS, John Y. Kwon, MD
Disclosure Information©2015 by The Orthopaedic Journal at Harvard Medical School
Open reduction and internal fixation using conventional and locked plates is the standard of care for femoral condylar fractures in an attempt to restore articular congruity. We report the use of a calcaneal plate as a novel technique for the fixation of a large medial collateral ligament avulsion fracture associated with a medial femoral condyle fracture. A calcaneal plate can be easily contoured to fit the femoral condyle, allows for fixation of fracture fragments by providing a washer effect and allows a wide array of screw placement options.
Unicondylar fractures of the distal femur are rare injuries accounting for less than 1% of all femoral fractures1, 2 and are partial articular fractures. The intact condyle is in continuity with the femoral metaphysis.3 These unusual injuries may be overlooked in the acute trauma setting considering they are often associated with other injuries in the ipsilateral extremity. Open reduction and internal fixation of unicondylar femur fractures is the accepted treatment of choice and provides overall excellent long-term results.4
Multiple fixation techniques have been advocated for fixation for articular fractures of the distal femur. Dynamic condylar screws, lag screw fixation as well as conventional and locked plates are the modalities commonly used for supracondylar fractures and fractures of the lateral femoral condyle. Most of the currently available femoral condylar plates are pre-contoured to the lateral femoral condyle. Hence fixation of medial femoral condyle fractures is amenable only to screw fixation or by the use of various plate options not specifically designed for this purpose.
We present a case of medial femoral condylar fracture,(AO [Arbeitsgemeinschaft für Osteosynthesefragen] classification 33-B2) fixed with a calcaneal plate. The patient provided written informed consent for print and electronic publication of the case report.
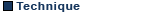
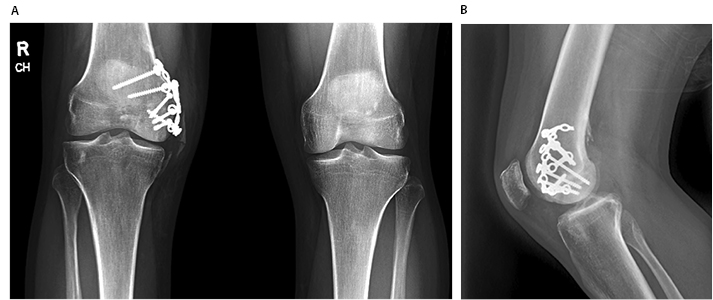
The patient is a 24 year old male who sustained an accident on a jet ski while on a cruise vacation injuring his right knee. He was subsequently transferred to our institution for further care. He complained of isolated knee pain, difficulties with range of motion and was unable to bear weight. Physical examination revealed a swollen, tender right knee with extensive ecchymosis. Range of movement could not be ascertained because of pain and he was neurovascularly intact. Radiographs revealed a fracture of the medial femoral condyle (Figure 1). Given the diagnosis of a displaced, intra-articular fracture of the distal femur, the decision was made to proceed with operative reduction and fixation.
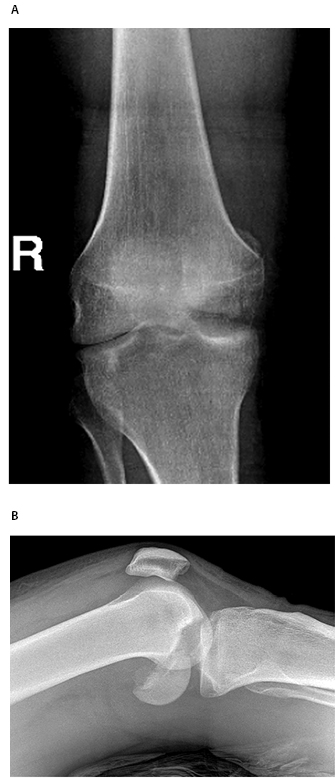
The patient was taken to the operating theatre and placed in the supine position. He was prepped and draped in normal sterile fashion. An antero-medial approach to the distal femur was performed. The vastus medialis was elevated anteriorly. The fracture hematoma was irrigated. The displaced medial femoral condyle was reduced and provisionally fixed in place with multiple 1.6mm K-wires after confirming articular reduction clinically and radiographicaly. K-wire joysticks were used to help guide the reduction, and a large pointed tenaculum was used to anatomically reduce and compress the primary fracture line. The medial femoral condyle was fixed using three 4.0mm partially threaded cancellous lag screws (Figure 2). Intraoperatively, a large sleeve of bone on which the medial collateral ligament was attached was identified that was not well appreciated on preoperative radiographs (Figure 3).


The medial avulsion fracture, which was comminuted into several fragments, was reduced and fixed in place with K-wires. In order to get a washer type of buttressing effect, a Synthes calcaneal locking plate (West Chester, PA) was contoured to sit flush against the medial femoral condyle. Excessive tabs were removed and the plate was fixed with multiple 4.0mm cancellous screws (Figure 4). After fixation was completed, ligamentous stability of the knee was assessed and there was no medial gapping noted with valgus stress. The wound was irrigated and closed in layers.
At six-month follow-up, the patient was weight-bearing as tolerated with knee range of motion from 0-100 degrees. He was doing well but reported stiffness to flexion and radiographs revealed the presence of heterotopic bone in the area of the MCL (Figure 5). A knee manipulation under anesthesia was performed shortly thereafter, and range of motion at final followup was 125 degrees of flexion with no extension lag. At 1-year follow-up he had no pain, had knee motion symmetric to the normal side and was able to perform recreational activities without difficulty. He reported no problems with the plate or plate prominence.
Open reduction and internal fixation is the treatment of choice for displaced distal femoral fractures. The primary goals of surgery are to restore articular congruity and anatomic alignment. Stable fixation of articular fragments allows for early knee motion which prevents stiffness and facilitates recovery.
In the absence of specific implants for the fractures of the medial femoral condyle, we used a calcaneal plate which appears to be a viable option for this kind of fracture pattern. Advantages of the calcaneal plate for this application include plate strength yet malleable nature, low profile and easy contour ability. This allows the calcaneal plate to be easily applied in a buttress fashion to the femoral condyle reducing the chance of prominent hardware. Multiple screw holes of the calcaneal plates allow various options of screw placement depending upon the fracture pattern. Hohman et al. described 2 cases in which calcaneal plates were utilized for the fixation of both medial and lateral condylar fractures.5
This technique of fracture fixation however is only indicated in unicondylar fractures. Complete articular fractures and those with metaphyseal comminution require different methods of fixation.