Original Submissions
Current Issue: Volume 15 | ![]() PDF
PDF
Syndesmotic Injuries: Is There a New Standard of Care? A Case Report and Commentary
John Y. Kwon, M.D., Mostafa M. Abousayed, M.D., Xavier Simcock, M.D.
Department of Orthopaedic Surgery, Massachusetts General Hospital, Harvard Medical School, Boston, MA 02114
Background
Diagnosis and treatment of syndesmotic injuries, whether associated with malleolar ankle fractures, Maisonneuve fractures or purely ligamentous injuries, has been extensively researched. There has been increasing interest as more recent studies have demonstrated a relatively high rate of syndesmotic malreduction and resultant morbidity after surgical fixation. These studies suggest the need for more advanced imaging studies both preoperatively and intraoperatively, as well as a change in traditionally used surgical techniques, to ensure optimal treatment of syndesmotic injuries.
Obtaining plain radiographs of the injured ankle followed by fixation of the syndesmosis using classically taught reduction techniques with intraoperative fluoroscopy to ensure proper reduction has long been the standard of care. However, the current evidence suggests that doing things the old way may be the wrong way.
We present an illustrative case report as well as a commentary based on the current literature.
Case Report
Patient CS is a 31 year old female who sustained a closed ankle fracture in October, 2012 treated with open reduction internal fixation at an outside institution. She presented to Massachusetts General Hospital for a second opinion given continued pain and swelling approximately 7 months after surgery. She complained of irritation from the lateral plates and screws as well as anterolateral pain, especially when planting and pivoting on her operated lower extremity. She underwent a course of physical therapy, bracing and NSAIDS without relief.
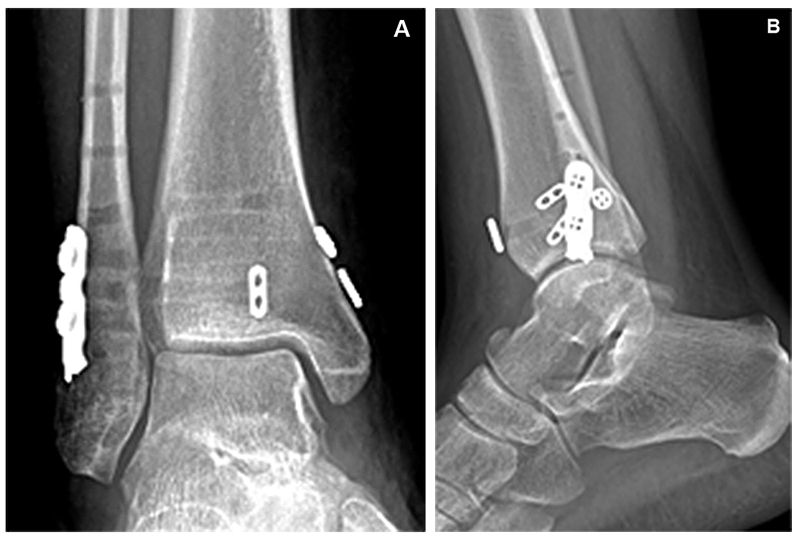
Physical examination revealed mild ankle swelling and well-healed surgical scars. She had tenderness to palpation over her fibular hardware, pain over the anterior syndesmosis and pain with external rotation stress testing. Plain radiographs revealed a healed ankle fracture with a lateral plate and screw construct with syndesmotic stabilization via a suture button device (Figure 1A, 1B). A CT scan of the ankle was obtained to assess syndesmotic reduction which confirmed malreduction secondary to posterior placement of the suture button device. (Figure 2) Given the patient’s pain, disability and continued failure of conservative treatment she was indicated for removal of hardware and revision syndesmotic fixation.

Preoperative plain radiographs (A) AP (B) Lateral
All Rights Reserved. Permission For Use Required.
-View Large-
Preoperative CT scan showing malreduced syndesmosis
All Rights Reserved. Permission For Use Required.
-View Large-
All Rights Reserved. Permission For Use Required.

All Rights Reserved. Permission For Use Required.
Intra-operative O-arm image after syndesmotic reduction and suture button fixation in a divergent fashion
The patient was seen 2 weeks postoperatively and was doing well. Sutures were removed, radiographs obtained and physical therapy initiated. The patient was made nonweightbearing in an aircast boot. She progressed her weightbearing at 6 weeks and had an uneventful recovery with improved function and decreased pain. (Figure 4A, 4B)
Post-operative plain radiographs
All Rights Reserved. Permission For Use Required.
-View Large-Discussion
Anatomical reduction of the syndesmosis is important for ankle stability and normal transmission of forces across the tibiotalar joint to minimize the incidence of posttraumatic arthritis.1-5 Kennedy, et al. demonstrated that even subtle malreduction of the syndesmosis resulted in increased focal pressures across the ankle joint with consequent ankle arthrosis.6 Similarly others have shown the rapid development of ankle arthritis at an average of 4 years following injury when the syndesmosis is malreduced.7 Recent literature has shown a relatively high rate of syndesmotic malreduction after surgical fixation and resultant morbidity. Gardner, et al. evaluated a cohort of 29 patients with ankle fractures who underwent surgical fixation with 52% demonstrating malreduction on postoperative CT scans.10 Miller, et al. similarly demonstrated close to 50% malreduction using traditional techniques in a cohort of 25 patients.11 Sanders, et al. recently published a two year follow-up of 68 patients with known syndesmotic malreduction after surgical fixation demonstrating statistically worse clinical outcomes when evaluated using the SFMA and the ankle specific Olerud/Molander questionnaires.31
As more outcomes studies demonstrate increased morbidity with syndesmotic malreduction, this calls into question our ability to detect proper anatomic reduction. Are plain radiographs (or fluoroscopy) adequate to assess accurate reduction? Traditionally, intraoperative evaluation of syndesmotic reduction is performed via fluoroscopy. However, both static and stress radiographs have been suggested to be unsatisfactory in multiple studies.23-27 Some studies have shown an average of 16% malreduction of the syndesmosis when reliant on plain films.28-30 There is also lack of consensus in terms of the radiographic parameters used as well as their accuracy. Marmor, et al. demonstrated in a cadaveric study the inability of traditionally used radiographic parameters such as tibiofibular clear space and overlap to accurately assess anatomic reduction, in particular for rotational malreductions. Gardner, et al. evaluated a cohort of 29 patients with ankle fractures who underwent surgical fixation. When comparing plain radiographs to axial CT scans obtained postoperatively, 6 (24%) cases were diagnosed with malreduction of the syndesmosis on plain films whereas, 13 (52%) revealed malreduction on CT scans.10 While some authors have advocated the use of post-operative CT to assess syndesmotic reduction, this is problematic as post-operative analysis requires a return back to the operating theatre when revision syndesmotic fixation is required.
Current evidence suggests that intraoperative assessment using CT-type imaging modalities that can produce axial imaging of the distal tibia-fibular joint is the most effective means of accurately assessing anatomic reduction.8-13 But what exactly is “anatomic” when imaging the syndesmosis using axial CTs? Dikos, et al. used axial CT scans to evaluate the normal anatomical variations in tibiofibular relationship. Not only did they find gender differences in certain anatomic parameters but they also found normal variation when a side-to-side comparison was performed. Despite this, they recommended using the patient’s contralateral ankle as a guide when assessing syndesmotic reduction rather than depending on predefined measurements.14 This was also reported in another study which recommended using comparative CT scans rather than plain images or single limb post-operative CT scan which were found to be of limited value when assessing syndesmotic reduction.15 These data not only suggest the need to image the contralateral uninjured ankle, but also challenge the absolute accuracy of using this technique to assess anatomic reduction of the injured side. Furthermore this calls into question whether the rates of malreduction as demonstrated by previous studies was truly as high as reported.
What about surgical reduction of the syndesmosis using traditional techniques?
Although a variety of methods have been described for reduction of the syndesmosis, indirect reduction using reduction forceps with verification using intraoperative fluoroscopy is most commonly performed.16-19 Traditionally, the forceps is placed obliquely, compression performed in the coronal plane with the ankle in neutral or slight dorsiflexion with fixation placed at 20-30 degrees from the horizontal due to the relative posterior anatomic position of the fibula compared to the tibia.20 But is this technique reliable for anatomically reducing the syndesmosis? Phisitkul, et al. found in their cadaveric study that there is an optimal place for forceps placement to achieve accurate reduction and stated that syndesmotic malreduction can be produced if the forceps was placed at different landmarks. They discovered a degree of over compression in all clamping alignments however; they mentioned that its clinical significance is unknown.21 Miller, et al. confirmed these findings in another study showing a high incidence of syndesmotic over-compression and malreduction. They demonstrated that for optimal reduction using the clamp forceps, it should be angled to 0° rather than 15° or 30° with the lateral screws directed at 0° and the posterolateral screws directed at 30° from the fibula in the coronal plane.22
If indirect reduction can lead to malreduction does open reducing the syndesmosis, ie directly visualizing the incisura, lead to anatomic reduction? Miller, et al. reported on open reduction of the syndesmosis. They compared a cohort of 149 patients who underwent open reduction of the syndesmosis to a previously treated group of 25 patients who underwent indirect fluoroscopy-assisted reduction. 24/149 (16%) in the direct visualization group were proven malreduced in postoperative CT scans in comparison to 13/25 (52%) in the control group. They further subdivided the direct visualization group into patients with posterior malleolar fractures who underwent ORIF regardless of the size of the fragment (including patients with ankle fracture-dislocations) and patients with purely ligamentous disruptions with syndesmotic screw fixation only. A trend toward significance was observed in the posterior malleolar group, which signifies the importance of anatomical reduction of the posterior malleolus.11 In another study, 68 patients were prospectively followed for a minimum of 2 years follow up. 2/13 (15%) who had open reduction were found to have malreduction when CT scan was performed (with comparison CTs obtained of the uninjured side) while 25/55 (44%) of the closed reduction group were proven malreduced.31 While open-reducing the syndesmosis appears to improve the odds of obtaining an anatomic reduction as compared to indirect reduction, the literature continues to demonstrate a relatively high malreduction rate even when directly visualizing the syndesmotic joint.
In summary, the current literature suggests that in order to ensure anatomic reduction and improve patient outcomes the treating surgeon should: (1) obtain a CT scan of the contralateral unaffected side for comparison while also accounting for anatomic variation, (2) utilize intra-operative CT to assess anatomic reduction, and (3) make alterations in classically taught reduction techniques. But at what cost? It seems unreasonable and cost-prohibitive to assess every surgical patient with a known or suspected syndesmotic injury in this manner but yet it is unclear which patients may require a higher level of assessment. Intra-operative CT is a modality that is not commonly available at most institutions and there exists a significant cost consideration. Furthermore there are practical issues to consider. While images are obtained relatively quickly using the O-arm (approx. 2 minutes per scan), operative time is increased due to positioning of the O-arm as well as image acquisition. In addition the radiation exposure is slightly increased as each scan using the O-arm produces approximately 7.9 mGy of radiation (roughly equivalent to 5.6 radiographs).
Is there a simpler solution to this problem? A new method for intra-operative assessment of syndesmotic reduction was reported recently by Summers, et al. which appears promising.37 They obtained mortise and lateral views of the contralateral uninjured ankle intraoperatively carefully examining symmetry of the clear spaces and lateral bony overlap. Following fixation, reduction was performed and confirmed using the contralateral ankle images as a template. This was immediately confirmed in the operating room with CT scan and if found to be malreduced, revision of the reduction was performed. 17/18 cases in their study showed anatomic reduction on CT scan. Only one case revealed syndesmotic malreduction and revision ORIF of the fibular fracture was done and resulted on anatomic reduction confirmed by a second CT scan.
More research needs to be performed to establish the most effective yet cost efficient method of assessing syndesmotic reduction given the poorer prognosis associated with syndesmotic malreduction. Imaging the contralateral uninjured ankle and open reducing the syndesmosis with judicious use of available advanced imaging modalities appears to improve outcomes.
References

