Original Submissions
Current Issue: Volume 15 | ![]() PDF
PDF
Spontaneous Dissociation of Prosthetic Humeral Head: A Case Report
Abigail N Byrne, B.A., Caitlin M McCarthy, B.A., and Laurence D. Higgins, M.D.
Sports Medicine Service, Department of Orthopaedic Surgery, Brigham and Women’s Hospital, Harvard Medical School, Boston, MA 02114
Abstract:Dissociation of a Morse taper arthroplasty is an uncommon occurrence, especially in the shoulder, reported in only one publication in the English literature.1 In response to reported dissociations of Morse taper modular humeral components, Blevins et al. identified conditions that would interfere with the Morse taper interface strength. The relevant cases were reported only in a single component design and occurred between 1988-1992. Subsequent reports of consecutive arthroplasties with this prosthesis failed to document further episodes of Morse taper dissociation.2
In contradistinction, dissociation of the femoral heads in hip arthroplasty has been more commonly reported.4,10-14 It most frequently occurs during reduction of a dislocated prosthesis that then needs to be surgically addressed. The dissociation is not always apparent on post-reduction radiographs, underlining the importance of scrutinizing the images for radiolucencies and the position of the head of the prosthesis in the acetabular cup.7
The present case pertains to a DePuy Global Advantage total shoulder prosthesis implanted in 2008. This prosthesis is a third generation anatomical model, unlike the 1988-1992 second generation component previously reported in the literature. Heretofore, there have been no cases of humeral head dissociation in third generation total shoulder prostheses.
The authors have obtained the patient’s informed written consent for print and electronic publication of the case report.
Keywords: dissociation, shoulder, arthroplasty, case report, metallosis, articulation
Case Report
A 65-year old female patient presented to our clinic three and a half years status post right total shoulder arthroplasty for rheumatoid arthritis. At the time of surgery, she underwent uncomplicated insertion of a DePuy Global Shoulder prosthesis, whereby the rotator cuff muscles were reportedly intact. She described pain and poor function of the shoulder since the procedure, with increasing pain and decreasing function over the preceding 8 months. The pain was reported as a 6/10 at rest to a 10/10 at its worst and awakened her from sleep; she reported a subjective shoulder value of 25%. Crepitus was noted during physical examination. The patient denied any inciting event or trauma.
Radiographs taken the day of the initial visit revealed dissociation of the humeral head from the humeral stem. The male component of the Morse taper appeared to be articulating with the glenoid component. CT revealed adequate glenoid bone stock, an asymptomatic os acromiale, and the dissociation of the Morse taper (Figure 1).

Plain films of the dissociated prosthesis at initial presentation
All Rights Reserved. Permission For Use Required.
-View Large-On physical examination, the patient demonstrated a pseudoparalytic shoulder with significant atrophy of the spinati muscles. There was marked tenderness to palpation over the proximal humerus at the site of the humeral component, with the appearance of the humeral component statically subluxed anteriorly and superiorly (anterior/superior escape). Range of motion on the affected side was less than 25° of forward flexion and abduction (Table I). The patient demonstrated a 20° lag in external rotation at 0° along with positive lift-off, bear hug and belly press tests, although examination was difficult due to pain. Furthermore, the patient has documented rotator cuff deficiency with tears of the subscapularis and supraspinatus.
Due to a variety of medical and family issues, the patient delayed surgical intervention despite her discomfort for a period of nine months. At her immediate pre-operative visit, radiographs confirmed persistence of the Morse taper dissociation.
The decision was made to proceed with conversion to reverse arthroplasty with transfers of the latissimus dorsi and the teres major tendons to improve function and diminish pain. Intraoperative findings included significant glenoid damage, resulting from articulation of the humeral male Morse taper component with the glenoid polyethylene component, including fracture of the polyethylene (Figure 2). Due to the prolonged period of dissociation, moderate metallosis and marked scarring were also found with resultant component instability (Figure 3). The humeral head had migrated to the posterior aspect of the shoulder, and the subscapularis, supraspinatus, and infraspinatus were noted to be deficient.
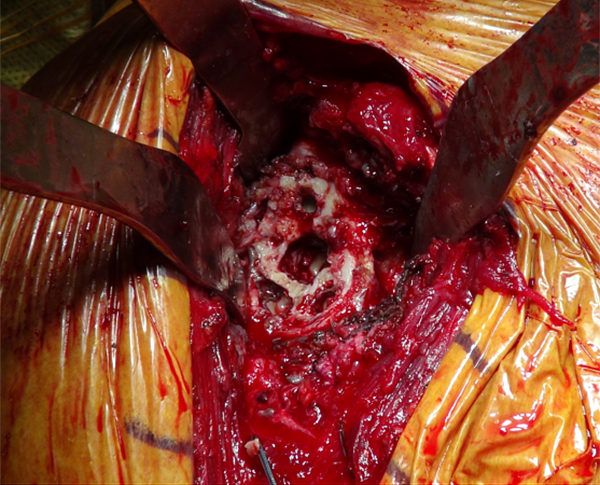
Deterioration of the glenoid bone stock due to articulation of male Morse taper component with glenoid polyethylene component
All Rights Reserved. Permission For Use Required.
-View Large-
Metallosis and scarring within articular space as observed during revision
All Rights Reserved. Permission For Use Required.
-View Large-Three months after revision, the patient was doing well without pain and actively engaged in physical therapy. She demonstrated forward flexion to 80° actively, and 150° passively with active external rotation to 45° bilaterally (Figure 4a-4b). Radiographs from the three month visit show a well placed reverse prosthesis without evidence of hardware complications (Figure 5a-5b).

Passive Forward Flexion, 3 months status post revision and conversion to Reverse Arthroplasty.
All Rights Reserved. Permission For Use Required.

External Rotation at 90º, 3 months status post revision and conversion to Reverse Arthroplasty
All Rights Reserved. Permission For Use Required.
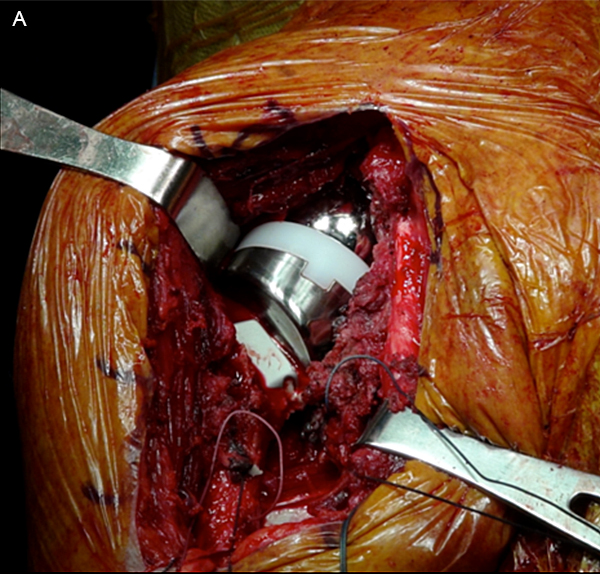
Revision and Conversion to Reverse Arthoplasty
All Rights Reserved. Permission For Use Required.
-View Large-
Plain films demonstrating well placed reverse prosthesis 3 months status post revision and conversion
All Rights Reserved. Permission For Use Required.
-View Large-Discussion
This case marks the first time in the literature that spontaneous dissociation of a humeral head in the third generation shoulder arthroplasty has been reported. It also represents a deviation from the literature on dissociation of a Total Hip Arthroplasty, which is often precipitated by a dislocation or other trauma. However, similar to cases of dissociations in the hip literature, this case was not caught at the onset of the patient’s discomfort. Consequently, the patient spent several months with a dissociated humeral head, leading to significant inflammation and metallosis. The metallosis itself is an unnecessary contributor to the patient’s prolonged discomfort.8 Additionally, the degree of metallosis and subsequent scarring necessitated extensive debridement, which, coupled with the loss of glenoid bone stock due to articulation of the humeral component, inherently limited the options for revision arthroplasty and may have a negative impact on the patient’s long-term functional outcomes.
Furthermore, metallosis itself has the potential for significant negative impact. A potential cause of polyneuropathy is cobalt-chromuim metallosis from hip arthroplasty.3 The long-term implications of debris from metal-wear were reviewed in 2007, pertaining to their potential toxicity, local and systemic implications, and influences on carcinogenesis.5 Although, as pointed out by Khan, et al., a causal relationship between orthopedics prostheses and toxic metal levels has not yet been demonstrated,6 and levels sufficient to be toxic are highly unlikely to be reached from deterioration of an implant, let alone metallosis.9 At best, metallosis is a localized inflammatory reaction of the periprosthetic bone and surrounding soft tissues in response to metallic debris. This inflammatory response is a common secondary complication in revision arthroplasty.
Conclusion
In the interest of patient outcomes in the face of a dissociated prosthetic humeral head, early detection is important. Careful inspection of radiographs is essential for identifying these cases. Early detection will hopefully preserve limited glenoid bone stock and prevent the development of significant metallosis. Early diagnosis and treatment may therefore improve patient outcomes.
References


