The Prevalence of Disordered Eating in a Sports Medicine Clinic Population: Implications for Multidisciplinary Care
Miho J. Tanaka, MD, Jared Forman, BA, Angela S. Guarda, MD, Lynne C. Jones, PhD, Sameer Dixit, MD
©2021 by The Orthopaedic Journal at Harvard Medical School
BACKGROUND Eating disorders have been associated with certain musculoskeletal injuries, yet their overall prevalence in sports medicine patients is unknown. We aimed to describe the prevalence of disordered eating in a sports medicine clinic and determine associated factors.
METHODS Using the 28-item Eating Disorder Examination Questionnaire (EDE-Q), we assessed the presence of disordered eating among patients presenting to a sports medicine clinic. EDE-Q scores ≥2.3 were considered “at risk” for disordered eating, and behaviors such as binge eating, purging and compulsive exercise were recorded. Linear, logistic, and multiple regression analyses were performed to assess relationships between patient factors (age, sex, sport level, body mass index [BMI], nature of injury) and EDE-Q scores.
RESULTS 340 responses were included in the study. 58 patients (17%) were at risk for disordered eating (8.5% of men, 24% of women). The at-risk group was older (mean age±SD, 43±12 years vs 37±12 years, P = 0.011) than the non–at-risk group and had a greater BMI (32±7.0 vs 27±6.1, P < 0.001). Women were three times more likely than men to be at risk (odds ratio, OR 3.4, 95% CI, 1.76, 6.60, P < 0.001). 98 patients (28.8%) reported at least one occurrence of subjective and/or objective binge eating, purging, or compulsive exercise in the prior 28 days.
CONCLUSION 17% of patients in our sports medicine clinic were at risk for disordered eating, with almost one-third of patients reporting abnormal eating-related behaviors within the previous 28 days. Further study is needed to understand the relationship between disordered eating and musculoskeletal injuries.
LEVEL OF EVIDENCE Level IV Case Series
KEYWORDS Eating disorder; injury; nutrition; orthopaedic surgery; sports medicine
The reported lifetime prevalence of anorexia nervosa, bulimia nervosa, and binge eating disorder, respectively, are estimated to be 0.9%, 1.5%, and 3.5% in women and 0.3%, 0.5%, and 2.0% in men.1 In athletes, however, the prevalence of eating disorders is much higher, at 6%–45% in women and 0%–19% in men.2 Elite athletes who participate in sports focused on leanness from an aesthetic or performance perspective have the highest rates of disordered eating,2-9 with one study reporting a rate of 42% among female athletes who participate in “aesthetic” sports, such as gymnastics and dance.9
The relationship between disordered eating and musculoskeletal injury is often described in the context of the female athlete triad, which consists of disordered eating that leads to metabolic and hormonal changes and subsequent amenorrhea/oligomenorrhea and osteoporosis/osteopenia.2,7,10,14 As reduced energy availability negatively influences bone health in both sexes, recent risk assessment tools for bone-stress injuries have been expanded and modified to include men.16 Traditionally, the considerations of nutrition and eating disorders within the field of sports medicine have been thought of as being limited to young women. However, recent evidence has also shown that the prevalence of anorexia nervosa may be highest among individuals aged 30–44, with binge eating disorders being most prevalent between the ages of 45–59.17
Disordered eating has been associated with musculoskeletal conditions such as stress fractures and tendinitis.18 Melin et al.19 reported that low energy availability can negatively affect muscle mass and neuromuscular function and can increase risk of injury or illness that may affect performance. The authors emphasized the importance of early intervention to identify and prevent secondary health consequences. In addition to musculoskeletal effects, eating disorders can lead to serious medical complications, such as cardiovascular disease, diabetes, and even death.1,20
Although specialized programs such as screening during preparticipation physical examinations21 and more recent development of clinical assesssment tools22 have improved awareness and diagnosis of disordered eating in young female athletes in the context of the female athlete triad, the prevalence of disordered eating and need for consideration among other patient populations with musculoskeletal concerns is unknown. As disordered eating has been associated with musculoskeletal conditions, the aims of our study were to describe the prevalence of disordered eating in patients presenting to a sports medicine clinic and to identify associated risk factors in this population.
This study was approved by our institutional review board (IRB00141802). During the 2017-2018 academic year, new patients presenting to the practice of 2 sports medicine specialists who treat patients exclusively with musculoskeletal conditions were asked to participate in this study. 603 new patients (53% female) with a mean age of 45±14 were eligible for this study. We included patients aged ≥18 years with the ability to read and write in English. We excluded patients <18 years of age, as well as those who completed too few questions to allow for accurate scoring of the survey (ie, missing >5% of questions in each subtopic) (107), for a total of 340 surveys included in the analysis.
Participants were asked to complete the Eating Disorder Examination Questionnaire (EDE-Q) at the time of their appointment. The EDE-Q is a validated, self-reported screening tool to detect signs of disordered eating.23 This 28-item survey consists of 4 subscales that address the key attitudes and behavioral features of eating disorders, including:
- Eating concern
- Restraint
- Shape concern
- Weight concern
Eating concern was assessed by questions such as:
Have you a definite fear of losing control over eating?
Restraint addressed restriction of intake by asking questions such as:
Have you been deliberately trying to limit the amount of food you eat to influence your shape or weight?
Shape concern addressed topics such as:
How dissatisfied have you been with your shape?
Weight concern was represented by questions such as:
Have you had a strong desire to lose weight?
Items are graded on a Likert scale of 0–6, with 0 denoting no instance of the questioned behavior regarding dietary habits and concerns and 6 denoting that the behavior happened every day during the previous 4-week period.
Also included in the EDE-Q are 6 free-text questions that allow responses for the number of occurrences (e.g., binge eating) during the past 28 days. Responses to questions were recorded about the frequency within the previous 28 days of:
- Objective binge eating
- Self-induced vomiting to control weight
- Laxative use to control weight
- Compulsive exercise as a means of controlling weight
The subscale score is the mean of the subcategory responses, with a higher score indicating a greater risk for disordered eating. The global score is the mean of the 4 subscores. A global score of ≥2.3 indicates risk for disordered eating (sensitivity, 83%; specificity, 96%; positive predictive value, 56%).23 In addition to EDE-Q scores, patient characteristics, including age, height, weight, and sex were recorded. Current sport level (e.g., collegiate, club, recreational) and nature of the patient’s current injury were queried as free-text options.
Mean EDE-Q total scores were calculated. Patients with a global score of ≥2.3 were considered “at risk,” and those with scores <2.3 were considered “non–at-risk” for an eating disorder on the basis of community norms for the EDE-Q.24-26 Each group was described and compared by age, sex, body mass index (BMI), and site of injury using 2-tailed t-tests and chi-squared tests. Because of the lack of inclusive norms, each group was categorized by sex for further analysis. Univariate logistic regression analysis was performed to test for significant associations of age, sex, and BMI with EDE-Q scores in this population. Multivariable logistic regression analyses were then performed using the risk factors with P values <0.05 on univariate analysis, with EDE-Q score as the output, and age, BMI, and sex as the input. All analyses were performed using JMP software (SAS, Cary, NC) and MedCalc (Ostend, Belgium). P values <0.05 were considered significant.
In total, 447 survey responses were received. We excluded 107 surveys with incomplete responses to demographic or EDE-Q questions, leaving 340 surveys (56% response rate). Of these, 187 (55%) were from women. The age of respondents was 38±13 (mean±SD) years. Regarding the site of injury, 144 respondents (42%) presented with a lower extremity concern or injury, 89 (26%) with an upper extremity concern or injury, and 11 (3.2%) with a head/neck/back concern or injury. Eight (2.4%) respondents had multiple areas of concern or injury, and 88 (26%) listed their concern as “unknown.” Current level of sport was recreational for 179 respondents (53%), collegiate for 18 (5.3%), club level for 15 (4.4%), semi-professional or professional for 4 (1.2%) and “other,” “none,” or no response for 124 (36%).
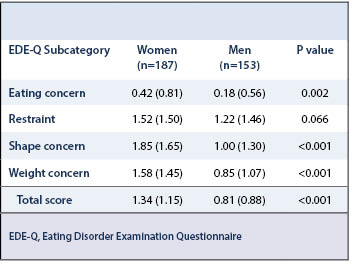
The mean EDE-Q score for the total study population was 1.10±1.07, with subset scores of 0.31±0.72 for eating concern, 1.38±1.47 for restraint, 1.46±1.56 for shape concern, and 1.25±1.34 for weight concern. Women had a significantly higher mean total score (P < 0.001) and mean subscores for eating concern (p = 0.002), shape concern (P < 0.001), and weight concern (P < 0.001) compared with men (Table 1). Forty-one patients (12%) reported undergoing extreme dietary restriction at least once during the past 28 days (more than 8 waking hours without eating to influence weight or shape). This included 20 women (11% of female patients) and 21 men (14% of male patients).
At-Risk vs Non–At-Risk Groups
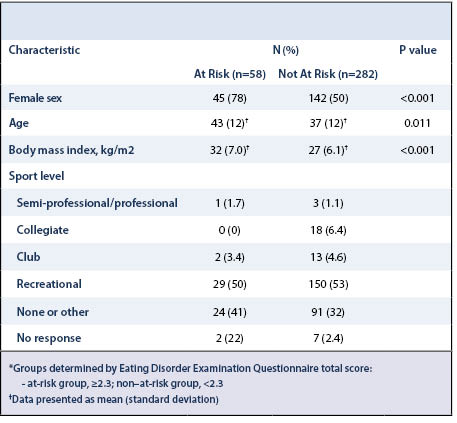
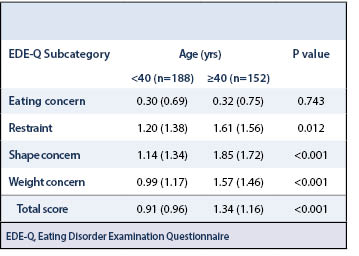
According to EDE-Q scores, 58 respondents (17%) were considered to be at risk for disordered eating. This group included 24% of women, and 8.5% of men (Table 2). Patients 40 years or older had significantly higher EDE-Q total scores, as well as higher subscores in restraint, shape concern, and weight concern (Table 3). The proportion of injuries or musculoskeletal concerns by body part did not significantly differ between the non–at-risk and at-risk groups. Both groups had similar proportions of patients who listed “unknown” for this section (26% vs 24%, P = N.S.).
Compared with the non–at-risk group, the at-risk group was older (P = 0.011), had a greater BMI (P < 0.001), and had a significantly higher proportion of women (P < 0.001). Women were significantly more likely than men to be classified as at risk according to total EDE-Q scores (odds ratio [OR] = 3.41; 95% confidence interval [CI]: 1.76, 6.60, R2 0.07, P < 0.001) as well as in the subsets of shape concern (OR = 2.80; 95% CI: 1.64, 4.75, R2 0.07, P < 0.001)) and weight concern (OR = 3.50; 95% CI: 1.93, 6.34, R2 0.09, P < 0.001).
Using the variables of age, BMI and sex, which were found to be significant in univariate analyses, multivariate analysis showed that female sex (OR = 3.17, 95% CI, 1.62, 6.23, P<0.001) and BMI>30 (OR = 2.59, 95% CI, 1.41, 4.74, P = 0.002) were independent risk factors for being at-risk based on total EDE-Q scores (R2 0.14, P < 0.001). The older age of the at risk group was not independently associated with EDE-Q score (OR = 1.66, 95% CI, 0.91, 3.06, P = 0.097).
Eating Behaviors
Questions regarding eating behaviors addressed those that occurred within the prior 28 days (Table 4). Ninety-eight patients (28.8%) reported at least one occurrence of subjective and/or objective binge eating, purging, or compulsive exercise in the prior 28 days. This included 58 women (31.0% of female patients) and 40 men (26.1% of male patients). Additionally, 102 (30%) reported overeating episodes in the prior 28 days, with males reporting this more commonly than females (34% versus 27%). Sixty-nine patients (20%) reported subjective and objective signs of binge eating, of whom 45 were women (24% of female patients) and 24 were men (16% of male patients). The number of those who had reported self-induced vomiting for weight loss or taking laxatives as a means of controlling weight in the prior 28 days were 1% and 2%, respectively.
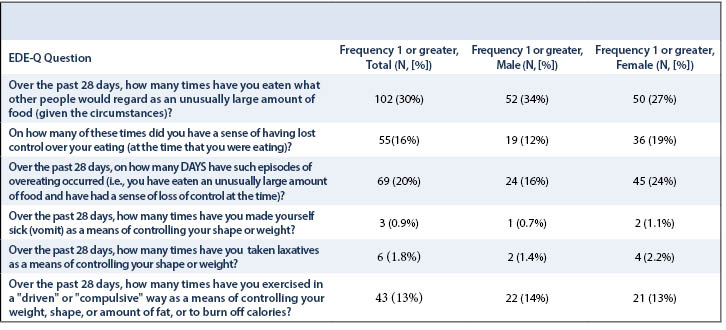
Forty-three patients (13%) reported compulsively exercising for weight loss, of whom 21 were women (13% of female patients) and 22 were men (14% of male patients). These patients reported “having exercised in a ‘driven’ or ‘compulsive’ way as a means of controlling your weight, shape or amount of fat, or to burn off calories” during the previous 28 days. Those who reported compulsive exercise were younger compared with those who did not report compulsive exercise (33±9.3 years versus 39±12.6 years, P < 0.001). However, no significant differences in BMI (27.5±5.4 vs 28.1±6.6, P = 0.539) or the proportion of injury types at presentation (47.6% lower extremity injuries vs 39.9%, P = 0.343) were found between the 2 groups.
In our cohort of patients with musculoskeletal injuries, 17% were found to be at risk for disordered eating. The at-risk group included 24% of female patients and 8.5% of male patients presenting to the sports medicine clinic. Studies have previously reported on the prevalence of disordered eating in specific populations such as athletes and women, describing a known relationship between disordered eating and certain types of musculoskeletal injuries involving stress fractures.14,27,28 However, to our knowledge, the prevalence of disordered eating in a general population of orthopaedic sports medicine patients with musculoskeletal concerns has not been described.
The prevalence of disordered eating in the general population is low, with norms typically reported according to age group and sex. In our study, 8.5% of men were considered at risk for disordered eating. Comparatively, normative data in a study of undergraduate male students reported mean EDE-Q score to be 1.1 (1.0), with a global score of 2.3 falling between the 85th and 90th percentiles.25 Another study of men who were middle-aged or older reported that 5% of the study population was considered at risk for disordered eating.29
In our study, 24% of the women seeking care for sports medicine injuries had an EDE-Q score ≥2.3. Although the prevalence of disordered eating is higher among women than among men, women in our study also had a higher prevalence than would be expected in the general population of women. In a Dutch study of 325 women, the authors reported that an EDE-Q score of 2.3 was in the 90th percentile for the general population;24 however, the same study reported that for a population of obese women without eating disorders, the same score of 2.3 would fall into the 30th percentile. This suggests that eating habits and norms can be influenced by multiple, patient-specific factors, and further studies are needed to identify which types of eating habits increase a patient’s risk of injury.
Despite the common belief that disordered eating is a young athlete’s disease, our study indicates that older patients may be equally, if not more likely, to experience symptoms of disordered eating. In our study, the at-risk group was older than those who were not at risk. This is in contrast to an epidemiologic study of >5,000 women, which found that global EDE-Q scores were significantly higher in ages 32 and below (1.56–1.59) when compared with the older age groups (1.41–1.42).26 However, Kummer et al.30 studied men aged 40–75 years in Austria and identified a significant association between eating disorder symptoms and symptoms associated with male aging. The authors recommended that physicians inquire about eating disorder symptoms in men aged ≥40 years. While multidisciplinary resources for disordered eating in the sports medicine community are currently directed toward young women,2,7,10,11,13,31 our results suggest that clinicians treating musculoskeletal concerns should be mindful of the increased rate of disordered eating in the older population.Although the global EDE-Q score reflects the overall severity of disordered eating, the subscales, particularly the restraint subscale, have been individually related to injury rates in prior studies. Nichols et al.7 compared female high school athletes with oligomenorrhea or amenorrhea versus those without menstrual abnormalities and identified a relationship between higher global EDE-Q scores (1.68±1.20 vs 1.33±1.14, P = 0.03) and restraint subscores (1.55±1.60 vs 1.04±1.27, P = 0.2). Rauh et al.14 further determined that female high school athletes with EDE-Q scores of 4.0 or higher on the restraint subscale were 7 times as likely to experience a musculoskeletal injury than those with scores <4.0. Furthermore, those with an elevated score in the shape concern subscale were 4.2 times as likely to experience injury as those with normal scores. The risks of injury based on elevated scores in the weight concern and eating concern subscales were significant as well, at 1.7 and 2.8 times higher than the risks for those with normal subscale scores, respectively. The authors reported that the most common sites of injury were the lower leg (33%, N=30) and the knee (21%, N=19). Overuse injuries accounted for 69% of all injuries, and acute injuries constituted 31%.
The relationship between symptoms of disordered eating and musculoskeletal injury in our study population is unclear. According to the analysis of responses regarding compulsive exercise, those who reported compulsive exercise habits were younger; whereas, those who were categorized as at risk for disordered eating were older and had greater mean BMI than the non–at-risk group. This makes it less likely that the musculoskeletal injuries in the at-risk population were related to increased activity level alone. In contrast, very little is known about the relationship between disordered eating and sports medicine injuries. While some metabolic and diet-related conditions have been shown to negatively affect tendon function or healing, further studies are needed to understand the influence of eating habits on orthopaedic conditions and treatment outcomes.32,33
One limitation of our study is that uninjured control patients were not included in this study, and therefore we were unable to compare eating habits to injury risk. Furthermore, specific injury diagnoses were not able to be studied. Because the diagnosis was reported by the patient instead of the clinicians, many responses were nonspecific or left blank, and the data could not be analyzed by injury type. The analysis of variables in this study were limited to the patient-reported factors listed in the survey and did not involve a priori selection of covariates that may have better described the relationship with EDE-Q scores. Additionally, we assumed that each patient in the sports medicine clinic had a concern of a musculoskeletal nature because both participating physicians have such practice types. Another limitation is that we used self-reported survey data and were therefore reliant on individuals answering truthfully about their eating habits. Although the EDE-Q is a validated survey, the addition of the Eating Disorder Examination interview in a formal evaluation could provide a more accurate representation of the level of disordered eating cognition and behaviors.
Overall, 17% of our patients seeking care for musculoskeletal concerns were determined to be at risk for disordered eating. These patients were more commonly female, were older, and had a greater BMI than those without signs of disordered eating. Furthermore, almost one-third of patients reported abnormal eating-related behaviors within the past 28 days. Our findings suggest that this type of pathology may be more prevalent in our patient population than previously described. Further studies are needed to examine the relationship between disordered eating with rates and types of musculoskeletal injury.
The authors acknowledge Kristin Veno for her assistance with obtaining demographic data for this study.