Does Sex Matter in Orthopedic Care?
Elizabeth Matzkin, MD, Caroline H. Hu, BS, Laura Bruse Gehrig, MD, Cordelia Carter, MD
The authors report no conflict of interest related to this work.
©2018 by The Orthopaedic Journal at Harvard Medical School
BACKGROUND Increasing scientific evidence establishes that sex-based differences (sexual dimorphisms) exist in common musculoskeletal conditions. The sex of the patient affected by a musculoskeletal disorder may have significant influence on that patient’s presentation, treatment course and ultimate clinical outcome. The purpose of this study was to evaluate the degree to which members of the American Academy of Orthopaedic Surgeons (AAOS) consider sex as a demographic variable during routine clinical and surgical decision-making.
METHODS An anonymous 10-question web-based survey was distributed to a randomly selected sample of 6000 AAOS members. This survey used a five-point Likert scale to determine orthopaedic surgeons’ self-reported behavior in evaluating and treating patients with common musculoskeletal complaints. Analysis of variance (ANOVA) tests with a 95% significance level were used to determine statistically significant differences amongst survey respondents.
RESULTS Three hundred forty-five AAOS members completed the online survey. Orthopaedic surgeons who had been in practice for less than 5 years and female orthopaedic surgeons were significantly less likely to routinely regard the sex of a patient as a factor during routine diagnosis and treatment plans than those surgeons who had been in practice longer or were male (p<0.05). Despite the fact that survey respondents generally disagreed with the statement that patient sex factors into treatment decision-making, they reported feeling well-prepared to recognize and care for patients with musculoskeletal disorders that are characterized by sexual dimorphism.
CONCLUSION Orthopaedic surgeons do not routinely consider the sex of a patient when evaluating and formulating treatment plans for patients with musculoskeletal disorders. Targeted attempts to provide early and ongoing education regarding sex-based differences in musculoskeletal disorders are likely necessary to address this knowledge gap.
LEVEL OF EVIDENCE Cross-sectional Study Level IV
KEYWORDSSexual dimorphism
Although it is widely understood that disease prevalence differs between men and women at a macroscopic level, it was not until the past decade that researchers began exploring sex differences at the cellular and genetic levels. In 2001, the Institute of Medicine released a landmark report titled Exploring the Biological Contributions to Human Health: Does Sex Matter?1 that concluded that there are significant unexplained differences in human disease between men and women and that research on sex differences needs to be promoted and expanded. The report defines “sex” as the “classification of living things, generally as male or female according to their reproductive organs and functions assigned by chromosomal complement”, and “gender” as a “person’s self-representation as male or female, or how that person is responded to by social institutions based on the individual’s gender presentation” and is shaped by environment and experience.1 In the scientific literature, the term “sex” should be used when differences are primarily biologic.
Beyond the cellular level, sexual dimorphism appears at the level of the muscle, bone, tendon and ligament. For example, women tend to have less muscle mass and different skeletal muscle fiber composition, with a larger proportion of Type I fibers that are more fatigue resistant than that of men.2 Additionally, sex-specific hormones such as estrogen and testosterone are implicated in muscle growth, regulation of muscle mass, and contractile function.3 Joint load is also influenced by muscle strength and fatigue and may differ between men and women. Women have lower bone mineral density and lower peak bone mass. Furthermore, female bone has less cortical area due to reduced periosteal apposition during growth, resulting in intrinsically weaker bone.4-66 Finally, functional stabilizing control also differs between men and women, because of sex-based differences in muscle recruitment and activation7-9 as well as greater ligamentous laxity amongst women.10-13
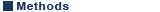
Given these anatomic, neuromuscular, and physiological differences, it is certainly plausible that sex might play a substantial role in musculoskeletal disorders and injuries. Numerous studies have indicated that chronic musculoskeletal diseases are more prevalent in women than in men.14-18 Sexual dimorphisms exist in many musculoskeletal problems (Table 1). Additionally, management of musculoskeletal disease might also be impacted due to sex differences in pain responses: research has shown that women are more able to discriminate pain due to different neural circuits and pain receptors.14,19 Different responses to various analgesics and anti-inflammatory medications have also been described for men and women.20-21
Orthopaedic surgeons should be aware of sex differences as they pertain to incidence, disease presentation, diagnosis and management of various musculoskeletal conditions. Recognizing these sex-related differences is critical to providing the best quality of health care. However, it is unclear whether existing sex differences in musculoskeletal health are well known within the orthopaedic community. This article presents the results of a nationwide survey among American Academy of Orthopaedic Surgeons (AAOS) members assessing knowledge of sexual dimorphisms in musculoskeletal health.
The primary hypothesis of this study is that orthopaedic surgeons do not generally take sexual dimorphisms in musculoskeletal disease into account when evaluating and providing care for patients. Secondary objectives of the study were to determine if female surgeons, those that have recently completed residency and/or fellowship training, and/or those that are domestic members of the AAOS are more likely to factor patient sex into clinical and surgical decision-making.
Study Population
A 10-question survey was designed to assess the extent to which patient sex is a contributing factor in the evaluation and management of patients with common musculoskeletal disorders (Appendix 1). The pilot survey was developed and reviewed by 15 members of the AAOS Women’s Health Advisory Board (WHAB). It underwent revision and, once finalized, was distributed in collaboration with the AAOS survey research office. Specifically, an e-mail containing a link to the survey web site was sent to 3000 Domestic and 3000 International AAOS members randomly selected by a computer program. Bi-weekly email reminders were generated automatically for those who had not completed the survey. Four weeks after initial distribution, data collection was concluded.
Survey Design
The first four survey questions sought to obtain basic demographic information including sex of the surgeon, number of years in practice, subspecialty field, and practice setting. Respondents were then asked to rate their level of agreement, using a 5-point Likert scale, with various statements regarding the role that patient sex plays in determining treatment decisions throughout the course of orthopaedic management from pre-operative evaluation to post-operative treatment (e.g., “The sex of my patient factors routinely into my pre-operative care and decision-making.”)
The remainder of the survey content was developed to specifically investigate treatment for patients with orthopaedic problems with well-established sex-based differences, such as hip fracture, ACL tear, and osteoarthritis of the knee. For each musculoskeletal disorder, study participants were asked about their level of agreement on a scale of 1 (strongly disagree) to 5 (strongly agree) with the statement, “The sex of my patient guides evaluation, diagnosis and management decisions for [orthopaedic problem]”.
Finally, the last question asked each participant to rate his/her level of agreement with the statement, “I feel well-prepared to recognize musculoskeletal disorders that are characterized by sexual dimorphism (e.g., different male and female presentations) and treat my patients accordingly,” on a scale of 1 (strongly disagree) to 5 (strongly agree).
Data Collection and Analysis
Surveys were completed anonymously; the AAOS software utilized returned completed survey data to the AAOS without any identifying information attached to it. Members of the AAOS Department of Research and Scientific Affairs then analyzed the data. Independent samples t-tests and analysis of variance (ANOVA) tests were used to determine statistically significant differences amongst survey respondents, with the significance level set at 95% (p≤0.05).
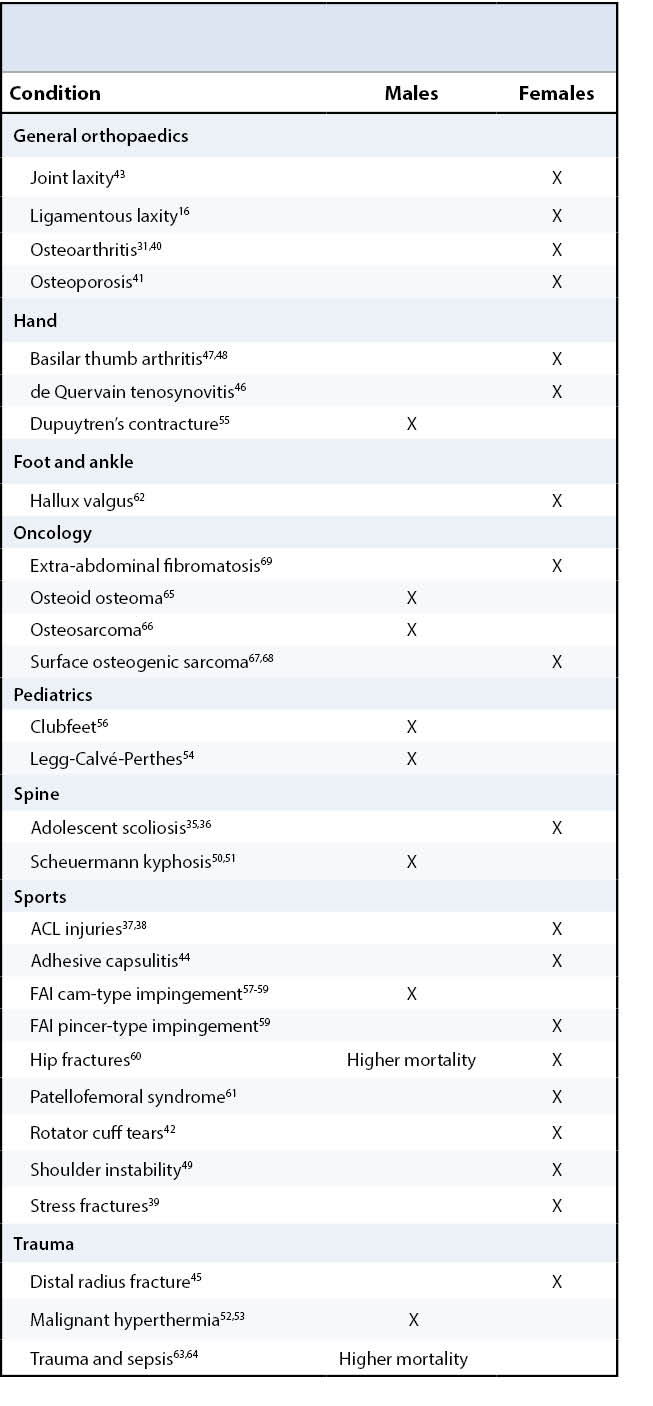
Of the 6000 invitees, 3000 were domestic AAOS members (based in the United States) and 3000 were international AAOS members. Three hundred forty-five members completed the online survey for a total response rate of 5.75%. One hundred twenty-nine domestic members responded (4.3%) and 216 international members responded (7.2%).
Demographics
Of the total respondents, 83% were male and 17% were female (Table 2). The largest group of respondents had been in practice greater than 25 years (37%). Residents and fellows made up the smallest percent of respondents (7%). The three most frequently reported subspecialties were general orthopaedics (21%), joint reconstruction (17%) and sports (13%). The three least frequently reported subspecialties were oncology (1%), spine (4%), and foot and ankle (5%). Just over half of respondents indicated an academic or hospital-based practice setting (52%), followed by private single or small group practice (22%) and private large group practice (17%).
Routine Care
Respondents were asked to report their level of agreement as to whether the sex of a patient routinely factors into overall care, pre-operative care and decision-making, surgical decision-making, and post-operative care and decision-making. Levels of agreement were determined using a scale of 1 to 5, with “1” representing strong disagreement and “5” representing strong agreement with a given statement.
The mean response score for whether patient sex routinely factored into his or her overall care was 2.55, meaning most orthopaedists report between slight disagreement and neutrality towards this statement. Significant differences were found based on years in practice and sex of the surgeon. Specifically, orthopaedic surgeons who had been in practice for 10-15 years (mean 2.74), 15-25 years (mean 2.58), and over 25 years (mean 2.71) all agreed that patient sex routinely factored into his or her overall care significantly more than orthopaedic surgeons who had been in practice for 0-5 years (mean 2.00, p=.0.01) Additionally, male orthopaedic surgeons (mean 2.61) reported more agreement with this statement than female orthopaedic surgeons did (mean 2.24).
On average, orthopaedic surgeons disagreed with or were neutral towards the statement that patient sex routinely factors into pre-operative care and decision making (2.53), surgical decision-making (2.46), and post-operative care and decision-making (2.46) without significant differences found amongst surgeon subgroups.
Specific Orthopaedic Diagnoses
The breakdown of how much the sex of a patient guides evaluation, diagnosis and management decisions for ten specific orthopaedic problems with established sexual dimorphisms is shown in Table 3. The orthopaedic problems for which orthopaedic surgeons were most likely to factor patient sex into decision-making were scoliosis (mean = 3.45), hallux valgus (3.24), and patellofemoral syndrome (3.20). The orthopaedic problems for which surgeons were least likely to factor patient sex into decisions were hip fractures (2.58), knee osteoarthritis (2.58), and Dupuytren’s disease (2.64).
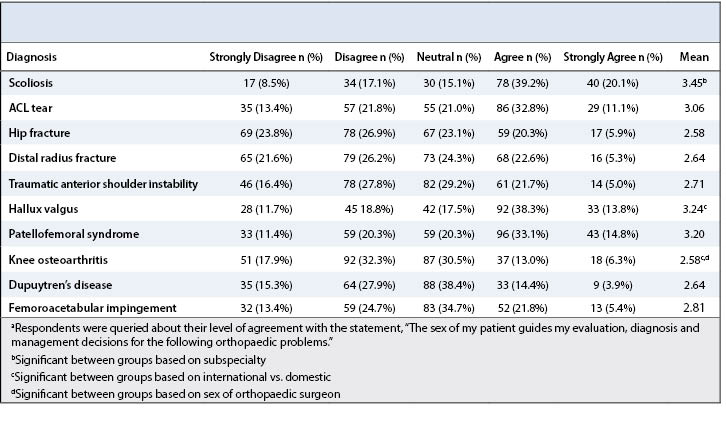
Significant differences were found for the impact of patient sex on evaluation, diagnosis and management for scoliosis based on subspecialty. Specifically, general orthopaedic surgeons, pediatric orthopaedists and spine surgeons were all more likely to take patient sex into account when treating scoliosis than were orthopaedists who reported specialization in hand, foot and ankle and oncology.
Among the other orthopaedic disorders studied, significant differences were found for hallux valgus and knee osteoarthritis. International orthopaedic surgeons (mean 3.36) were more likely to account for the sex of the patient in hallux valgus treatment than domestic orthopaedic surgeons were (mean 2.91, p=0.011). International orthopaedic surgeons (mean 2.67) were also more likely than domestic surgeons to take sex into account for knee osteoarthritis (mean 2.38, p =0.035).
Furthermore, male orthopaedic surgeons (mean 2.63) were significantly more likely to factor patient sex into evaluation, diagnosis and management of knee osteoarthritis than female surgeons were (mean 2.22 , p=0.036).
Self-evaluation
Overall, orthopaedic surgeon respondents agreed that they are well-prepared to recognize musculoskeletal disorders that are characterized by sexual dimorphism and to treat their patients accordingly (mean Likert score = 3.52). No significant differences were found based on sex of the surgeon, years in practice, subspecialty, practice setting, or type of AAOS membership (domestic or international).
In 2014, the NIH unveiled a new policy to monitor sex and gender inclusion starting at the preclinical research level by requiring report of balanced male and female cell lines and animals in future applications.22 A 2014 Journal of Bone and Joint Surgery (JBJS) editorial encouraged researchers to consider potential sex differences by aiming for inclusion of all populations at the clinical level and by providing sex-specific data.23
Our survey suggests that patient sex does not yet play an important conscious role in overall care, especially among younger orthopaedic surgeons, despite the recent push for advancement of knowledge of sex differences in musculoskeletal care. Surgeons who are 0-5 years into practice were significantly less likely to take sex into account into a patient’s overall care. Although orthopaedic surgeons who are 0-5 years into practice completed their medical school and residency training during the last ten years following the 2001 IOM report, it is clear that more needs to be done to translate knowledge on sex differences into clinical practice. Education on musculoskeletal sexual dimorphisms needs to be addressed at the medical school and residency training levels.
We had expected that female orthopaedic surgeons might consider patient sex as a factor more often because most musculoskeletal issues that have sex differences are more prevalent in women. However, our results demonstrated that men were significantly more likely than women to take patient sex into account in overall care.
Sexual dimorphism in several orthopaedic issues has been well documented in the literature.24 However, the majority of mean scores for whether patient sex guides evaluation, diagnosis, and management decisions are between “neutral” and “disagree”, even for issues that clearly have sex differences. Our data substantiates the hypothesis that orthopaedic surgeons are widely unaware of sexual dimorphism in musculoskeletal issues.
Over twenty years ago, Felson et al. showed that women develop knee osteoarthritis more frequently than men do.25 Women lose patellar cartilage more than twice the annual rate of men in patients with symptomatic knee osteoarthritis.26 Women have worse function and pain before total knee arthroplasty (TKA), as well as poorer function and pain following TKA for osteoarthritis.24-27 Furthermore, women may be less willing to undergo surgery or are more likely to delay surgery.24,28 Given the abundant research supporting sexual dimorphism in knee osteoarthritis, the sex of a patient should play an important role in clinical decision-making.
With a higher proportion of women in the US population coupled with a higher life expectancy among women, musculoskeletal sexual dimorphisms will factor more frequently into clinical decision-making in future orthopaedic practice. Knee osteoarthritis has well-described sexual dimorphisms; application to other areas of musculoskeletal medicine such as ACL injuries and fragility fractures will become increasingly relevant. Interestingly, in our study, the mean score for whether orthopaedic surgeons took patient sex into account for knee osteoarthritis was between “disagree” and “neutral” (2.58). Moreover, male orthopaedic surgeons were significantly more likely to factor in patient sex than female orthopaedic surgeons were during care for a patient with knee osteoarthritis.
The majority of mean scores for specific orthopaedic issues were between “disagree” and “neutral”, indicating that surgeons were not taking patient sex into account in clinical decision-making. Interestingly, however, the mean score for whether respondents felt well-prepared to recognize musculoskeletal disorders that are characterized by different male and female presentations and treat them accordingly was fairly high (3.52). This suggests that there is a disconnect between clinical practice patterns and how surgeons feel about the care that they are providing. Despite mounting evidence that patient sex should play a role in clinical decision-making, surgeons generally do not take sex into account. Yet surgeons are fairly confident in their abilities to recognize sexual dimorphism in musculoskeletal issues. This implies that knowledge regarding sex-specific differences in orthopaedic conditions is not being translated into clinical practice and that surgeons are unaware of this gap in translation.
Several limitations exist in this study. The first is the survey’s low response rate of 6%. According to AAOS data, response rates for AAOS survey studies are usually between 10-20%. Survey response rate varies based on the survey topic and the timing of the survey. Second, although the survey was distributed to a random subset of AAOS members, over half of respondents practiced in academic or hospital-based settings. Respondents in academic settings are more likely to be involved in research and thus, might be more likely to participate in a research survey or be more aware of recent literature regarding sex differences in orthopaedics. Additionally, since the survey was voluntary, respondents who chose to participate in the survey might be more concerned with sex differences in their practice compared to the general population. Lastly, due to the limitations of many analyses performed in this study checking for significance across many comparisons and subgroups, future studies to confirm findings should be performed. The true awareness of sex differences may be different in a larger sample size or in the general population.
Several aspects of these results warrant further research. An area of further investigation would be to determine whether younger orthopaedic surgeons are less likely to consider patient sex during clinical management due to a lack of sufficient training in sex-specific differences in musculoskeletal health. This could be explored by conducting an analysis of medical school curricula and residency education on sexual dimorphism in musculoskeletal issues. Future directions might include designing and incorporating modules on sex differences into existing musculoskeletal medicine curriculums. Our data suggests that medical students and residents are an important population to target for dissemination of sex-specific differences in orthopaedic issues and how these differences translate into practice.
In summary, the goal of this study was to determine the extent to which the sex of a patient plays a role in clinical decision-making for practicing orthopaedic surgeons. Our findings are consistent with our hypothesis that orthopaedic surgeons may be unaware of sexual dimorphism in musculoskeletal issues and that surgeons do routinely consider patient sex in their evaluation, diagnosis, and management decisions. It is concerning that respondents were confident in their ability to recognize musculoskeletal issues characterized by sexual dimorphism, but typically did not consider sex for these issues in their clinical practice. Our results highlight a gap in knowledge related to differences in health processes between men and women and their implications for clinical practice. Research on sex-specific differences in orthopaedic issues has not been disseminated to clinical audiences sufficiently, and this needs to be addressed. Understanding the differences and similarities between men and women in musculoskeletal health, including musculoskeletal development, is critical to making sex-appropriate diagnoses, treatment plans, and prevention strategies. It would be important to put greater effort and more resources into the promotion of awareness of sex differences in orthopaedic conditions in order to optimize patient care. This is critical as the population ages, people live longer, and remain active longer. Women make up greater than 50% of the population.
We recommend that education on musculoskeletal sexual dimorphisms be improved at the medical school and residency training levels. If addressed, an understanding of sex differences in musculoskeletal health will enable all physicians, especially orthopaedic surgeons, to treat each patient with specific biologic needs in consideration.