Bilateral Posterior Shoulder Fracture Dislocations after Generalized Seizure Managed with Open Reduction and Internal Fixation and Hemiarthroplasty: A Case Report
Arvind von Keudell, MD, Kempland C. Walley, BsC, Jaiben George, MS, Joseph P. DeAngelis, MD, Edward K. Rodriguez, MD, PhD, Paul T. Appleton, MD
The authors report no conflict of interest related to this work.
©2016 by The Orthopaedic Journal at Harvard Medical School
CASE We report on a patient with a history of lung cancer and bilateral posterior fracture dislocations of the glenohumeral joint due to seizure activity. A screw and plate fixation was performed for one shoulder whereas the other shoulder was treated with a hemiarthroplasty. At two-year follow-up, the patient had almost full range of motion with a good functional outcome in both upper extremities.
CONCLUSION The case presented raises the importance of holding a high index of suspicion for diagnosing bilateral posterior shoulder fracture dislocations in a patient with seizure activity. We discuss the various surgical and nonsurgical treatment options.
Posterior shoulder dislocations are the most commonly missed major joint dislocation.2 These cases are diagnosed late, if not missed entirely, due to ambiguous external signs and symptoms, coupled with the lack of proper imaging. Posterior dislocations are rare and account for less than 5% of all glenohumeral dislocations.1 The importance of identifying this condition relates to the patient’s poor clinical outcome when the diagnosis is delayed.2 Convulsive seizure activity has been associated with posterior shoulder dislocations, mostly resulting from powerful contractions of the lattissimus dorsi, pectoralis major, subscapularis, and teres major of the shoulder that can dislodge the humeral head from the glenoid fossa.
There have been several case reports on bilateral posterior glenohumeral dislocations, and reports indicate one side may be easily missed as a result of the difficulty in interpreting imaging, as well as the immediate focus on treating the seizure by emergency staff.1,3-16 In the absence of timely orthopedic care, patients may suffer from debilitating sequelae, such as loss of range of motion and increased incidence of avascular necrosis of the humeral head leading to poor long-term outcomes.17 Apart from a timely diagnosis, the various surgical treatment options for this condition are unclear due to its inherent infrequency, and basic concepts are usually transferred from outcomes on anterior shoulder fracture dislocations.18
We present a case of a 52-year-old man with bilateral posterior shoulder fracture dislocations following a generalized seizure who underwent immediate open reduction and internal fixation of the right shoulder. A closed reduction of the left shoulder was attempted in the operating room. Due to the comminution of the fracture, the left shoulder remained highly unstable. He was placed in a sling. Subsequent radiographic evidence confirmed posterior subluxation of the shoulder, and it was treated surgically with a hemiarthroplasty ten days after the initial injury.
A 52-year-old man with a history of lung cancer was brought to the emergency department after being found unresponsive in his apartment. Head Computed Tomography (CT) and cerebrospinal fluid (CSF) analyses were normal. A Chest CT was performed to assess for an intra-throacic disease process. He was emergently intubated for airway protection and the orthopedic trauma service was consulted after imaging revealed fracture-dislocations of bilateral shoulders.
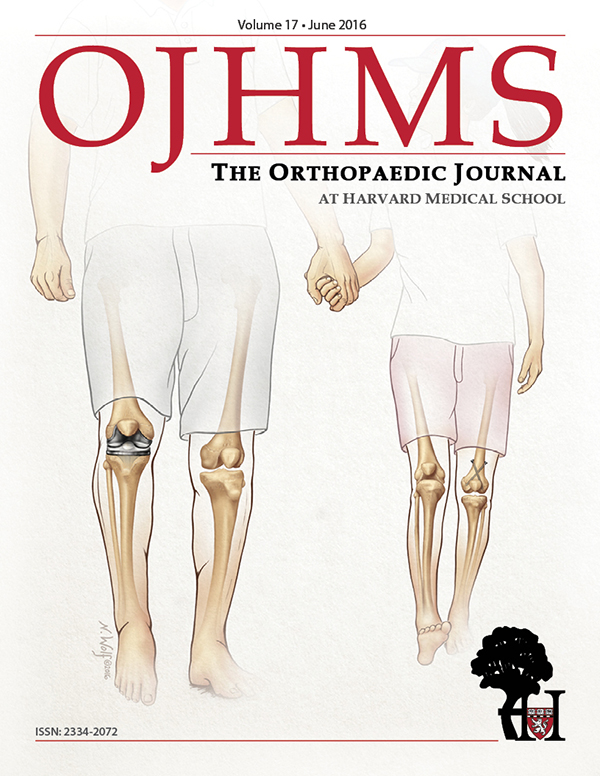
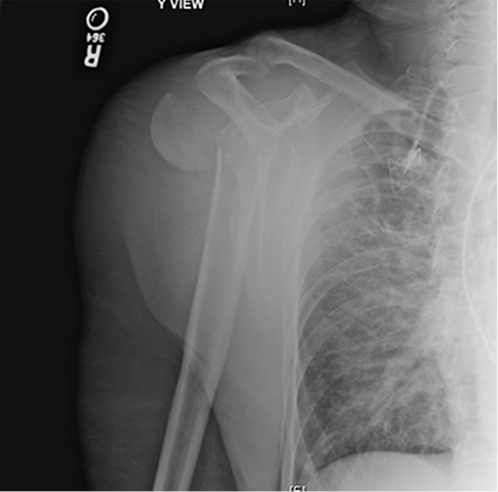
Plain radiographs showed a posterior fracture-dislocation of the right shoulder (Figure 1) and an impacted humeral head fracture of the left shoulder (Figure 2). A CT of the both shoulders was obtained for pre-operative planning.
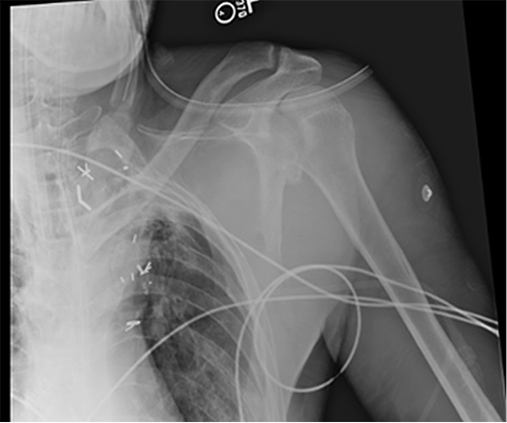
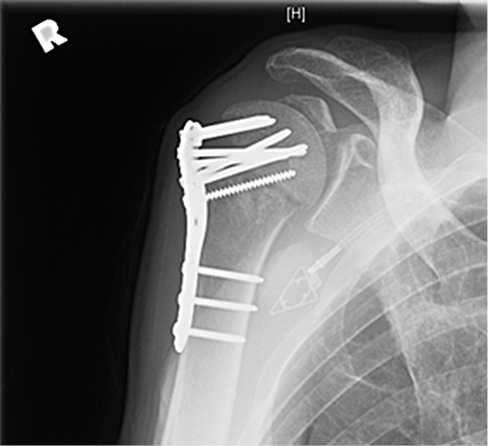
The patient was taken to the operating room once stabilized and he was deemed medically apporpirate for open reduction and internal fixation (ORIF) of the right shoulder. With regards to the left shoulder, a decision was made to leave the left humeral head perched onto the glenoid owing to its large reverse Hill-Sachs lesion for a possible hemiarthroplasty at a later date. The right shoulder was addressed through a deltopectoral approach. The head was gently reduced followed by fracture fixation (Figure 3) with a 3.5 mm locking compression plate system (Synthes, Paoli, PA, USA). Post-operatively, both shoulders were immobilized until the two-week follow-up mark. Passive range of motion and gentle pendulum exercises were started in the first week for the right shoulder. Given the size of the reverse Hill-Sachs lesion, the left shoulder was managed with a press-fitted hemiarthroplasty ten days after the injury (Figure 4).


Six weeks after the initial trauma, the patient was doing relatively well having returned to his previous level of work at a desk job, and regaining overall shoulder function. He had reported that his pain has been relatively well-controlled and denied any sensory deficits. He acknowledged occasional stiffness. Examination of his right shoulder demonstrated limited range of motion: with his elbow at his side, he had 20 degrees of external rotation, internal rotation to his abdomen. Examination of the left shoulder, which underwent hemiarthroplasty, demonstrated passive external rotation of 20 degrees, forward flexion of 120 degrees and abduction of 120 degrees.
Radiographs six weeks following hemiarthroplasty showed a left shoulder in good overall alignment without periprosthetic fracture or lucency (Figure 5). Plate and screw fixation of the right humeral neck fracture was identified without loosening. Signs of avascular necrosis were not observed at the initial follow-up visit (Figure 6).

The patient was contacted close to two years following the trauma, and his health care proxy (HCP) was able to comment on his physical function. His HCP reported minimal pain with rigorous activity, no sensory deficits, and frequent stiffness due to lack of physical activity resulting from cancer-induced fatigue. His DASH score was 10.8, ASES Shoulder Score was 76.7, and Mayo Elbow Performance Score was 75.
We present a case of bilateral posterior shoulder dislocations in an unconscious patient. In the absence of any clinical signs in a patient who experienced convulsive seizure activity, it remains of utmost importance to have a high index of suspicion for posterior shoulder dislocation. A generalized convulsive seizure is the most common cause of bilateral posterior shoulder dislocations.1,3-6,9,10,14,16,19-21 This finding is considered to be pathognomonic of a previous seizure episode warranting investigations for an underlying neurological disorder or possible electrocution. In rare cases, a strong convulsion may follow an electric shock or high-energy trauma; this is commonly referred to as the Triple E syndrome (epilepsy or any convulsive seizure, extreme trauma and electric shock). Shaw et al.5 proposed a possible mechanism for this kind of injury which typically occurs in the position of adduction, internal rotation and flexion. In this mechanism, the humeral head is forcibly internally rotated by severe contraction leading to the dislocation of the head over the glenoid rim posteriorly. Apart from trauma to the glenoid and labrum, posterior dislocations are often associated with an impaction fracture of the anteromedial humeral head, called a reverse Hill-Sachs lesion.22 It has been reported that a reverse Hill-Sachs lesion results in up to 86% of cases following a first-time traumatic posterior shoulder dislocation.22 Further injury may result in comminuted fractures of the proximal humerus as a result of the aggregated forces from the muscles that insert at the humeral head.
When these patients present with convulsive seizures, their emergent care often focuses on their neurological symptoms and can increase the likelihood that concurrent injuries may be overlooked. Anterior-posterior (AP) and oblique radiographs of the shoulder are easily misinterpreted and have low sensitivity when compared with axillary view or a CT scan. It is important to look for hallmarks of posterior shoulder dislocations like the light bulb sign (internally rotated humeral head appears rounded), trough line sign (a vertical dense line in the medial humeral head), or loss of overlap of the glenoid and the humeral head, because the axillary view is difficult to obtain in an injured patient. Delayed diagnosis may result in recurrent instability or the development of osteoarthritis and/or avascular necrosis. Furthermore, cases that require ORIF demonstrate inferior clinical outcomes.13 When the diagnosis is delayed more than three weeks after the inciting trauma, closed reduction is almost impossible and surgical treatment is recommended.14
The treatment of bilateral posterior shoulder dislocations depends on the duration from injury, the presence of associated injuries, the condition of the humeral head, the patient’s age and their functional demands.
Considerable debate remains regarding the preferred treatment for anterior or posterior shoulder fracture-dislocations. Some authors recommend ORIF in younger patients to preserve the humeral head while accepting the risk of avascular necrosis.18 When a reverse Hill-Sachs lesion is present, careful consideration of the humeral head’s anatomy is necessary. If the defect involves less than 25% of the articular surface, additional procedures may be avoided. Larger lesions warrant treatment to restore shoulder function and to prevent recurrent posterior instability when the humerus is internally rotated. Depending upon the presentation, various techniques can be employed to address the anterior bone loss. In younger patients, osteoarticular allograft bone grafting, lesser tuberosity transfer (McLaughlin procedure), or rotational osteotomy may help provide stability.23-27 For very large lesions involving greater than 50% of the articular surface, shoulder arthroplasty has been advocated.25,28
Hemiarthroplasty has been reported to provide a successful outcome in elderly patients, as it mitigates the risk of reoperation and the risk of avascular necrosis.25,28 Total shoulder replacement should be considered when there is extensive damage to the glenoid or pre-existing osteoarthritis.28 Reverse total shoulder arthroplasty has been more recently advocated for patients with a rotator cuff disease, even though long-term results remain sparse.29 Complications of shoulder arthroplasty, such as stem loosening, instability and infection may compromise long-term outcomes.30
In elderly patients with limited mobility and those who are at high risk for surgery, a conservative approach (benign neglect) may be utilized. In cases where the humeral head is intact, closed reduction with immobilization is the preferred treatment choice, though the position of the arm during immobilization is debated. If closed reduction is unsuccessful, operative treatment is required to locate the humeral head and to ensure stability.
In conclusion, in patients with seizure activity the treating physician should maintain a high index of suspicion for posterior shoulder dislocations. Urgent closed reduction should be the initial treatment goal. Various surgical treatment options exist and are generally reserved for patients with unsuccessful closed reduction and associated proximal humerus fractures.