Proprionibacterium acnes Infection Complicating the Operative Treatment of Clavicle Fractures
Arvind G. von Keudell, MD, Sandra B. Nelson, MD, Jesse B. Jupiter, MD
Disclosure Information©2015 by The Orthopaedic Journal at Harvard Medical School
BACKGROUND Management of failed surgical fixation of clavicle fractures resulting in nonunion is a challenging entity and warrants suspicion for indolent infection. Propionibacterium acnes (P. acnes) and other Proprionibacterium species have been recognized as one of the major sources of infection of the shoulder girdle. This study reviews a series of patients diagnosed with P. acnes infection after nonunion of a surgically treated clavicle fracture.
METHODS From 2002 to 2014, six patients were diagnosed with P. acnes infection after a failed surgical fixation of a clavicle fracture and were retrospectively analyzed. Clinical outcome was measured using pre- and post-operative outcome scores.
RESULTS All patients had an initial diagnosis of clavicle fracture that was treated with open reduction and internal fixation (ORIF). Four patients subsequently developed chronic nonunion and wound cultures revealed P. acnes at the time of revision ORIF or irrigation and debridement and were subsequently treated with intravenous antibiotics followed by a course of oral antibiotics. Two patients developed an acute infection after clavicle fixation within 3 months of the initial fixation and went on to nonunion. All six patients ultimately demonstrated union and had significantly improved physical function and reduction of pain.
CONCLUSION Failure of surgical fixation of clavicle fractures resulting in nonunion should raise suspicion for infection and cultures should be obtained. P. acnes has been recognized as a source of infection in the shoulder girdle; when recognized and treated appropriately, excellent functional outcome and union can be achieved.
Clavicle fractures represent a common injury of the shoulder girdle.14 Various treatment options have been proposed, ranging from nonsurgical treatment with a sling to surgical treatment using a variety of forms of internal fixation depending on location of the fracture. McKee et al.13 conducted a meta-analysis analyzing the current evidence of operative versus nonoperative treatment of displaced midshaft clavicular fractures. Operative treatment was found to result in earlier return to function, a reduced rate of nonunion, and an overall decreased complication rate when compared to nonoperative treatment. The complication rate (including nonunion, symptomatic malunion, infection, hardware removal, neurologic symptoms and refracture) was reported to occur in 29% in the operative group versus 42% in the nonoperative group. Postoperative pin site or wound infections occurred in 4% (9 of the 212 patients) treated operatively.
In the past decade, Proprionibacterium acnes (P. acnes) has been recognized as one of the major sources of infection after surgical interventions around the shoulder girdle.17 This study reviews a series of patients who were either from our institution or referred to our institution and diagnosed with P. acnes infection after either chronic nonunion or acute infection of a surgically treated clavicle fracture. The primary goal is to report on (1) radiographic union and (2) clinical outcome (Quick DASH, VAS and Range of motion) after the various treatment options applied for infection control or eradication of infected clavicle nonunions. Further goals are to (3) report on re- operations and (4) complications of all treated patients. Three exemplary cases will be discussed in further detail.
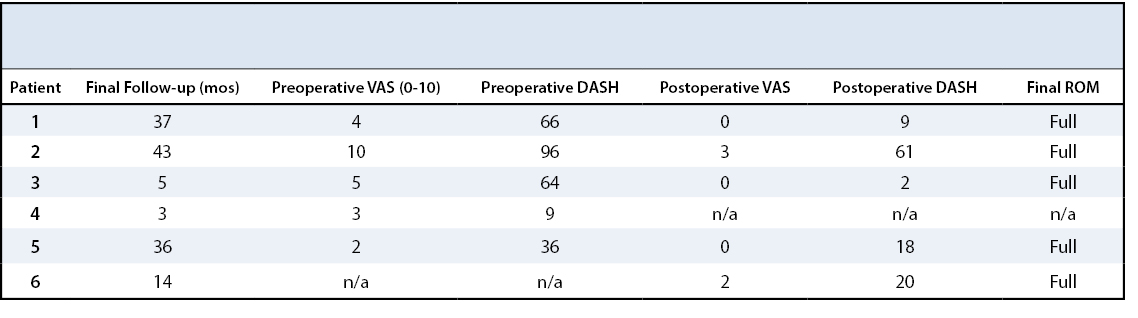
This case series was approved by the institutional review board. We retrospectively reviewed all patients seen for infections after surgically repaired clavicle fractures and treated at the Upper Extremity or Orthopaedic Trauma Department. Additionally, patients were identified using the Infectious Disease Outpatient Parenteral Antimicrobial Therapy registry. The retrospective review identified six patients who were treated between January 2002 and April 2014 (Table 1). Clinical outcome was measured by radiologic outcomes as well as patient rated factors including Quick DASH Score,3 Range of motion and Visual Pain Analogue.
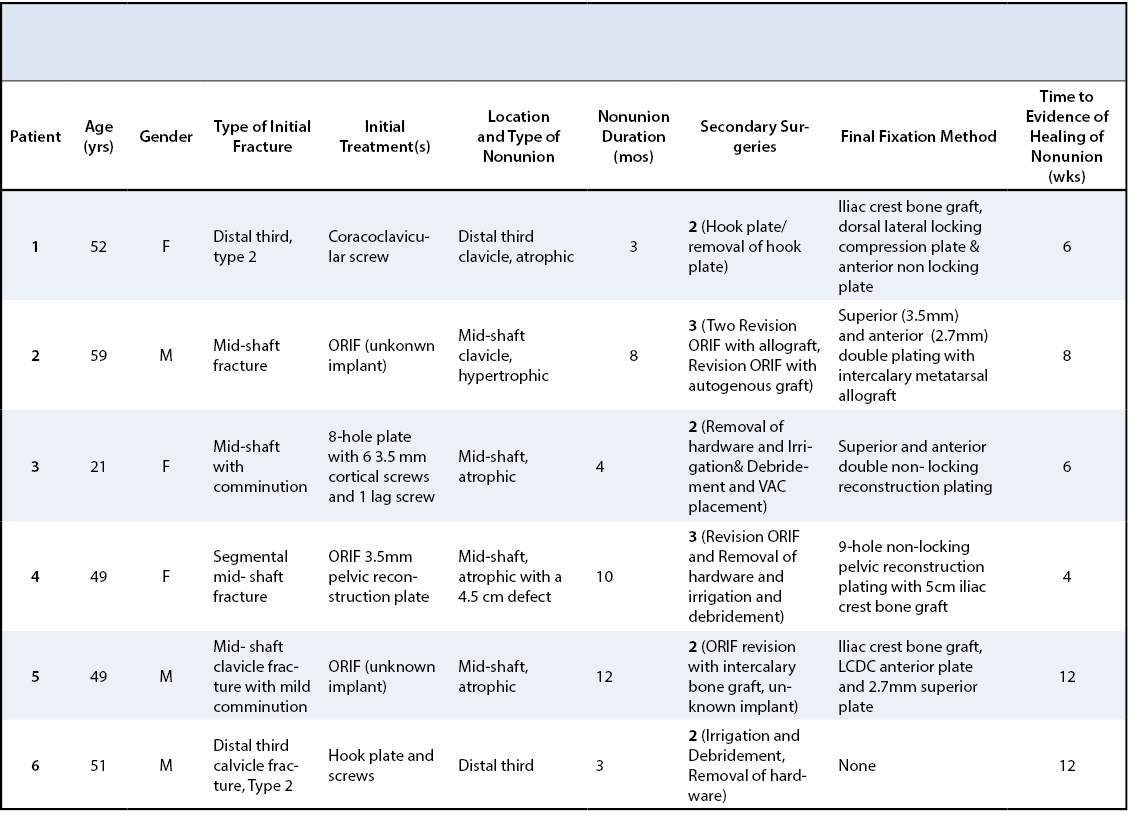
Four patients presented with a diagnosis of a nonunion of a clavicle fracture following surgical treatment and two patients developed acute infection following primary fracture fixation at our institution.
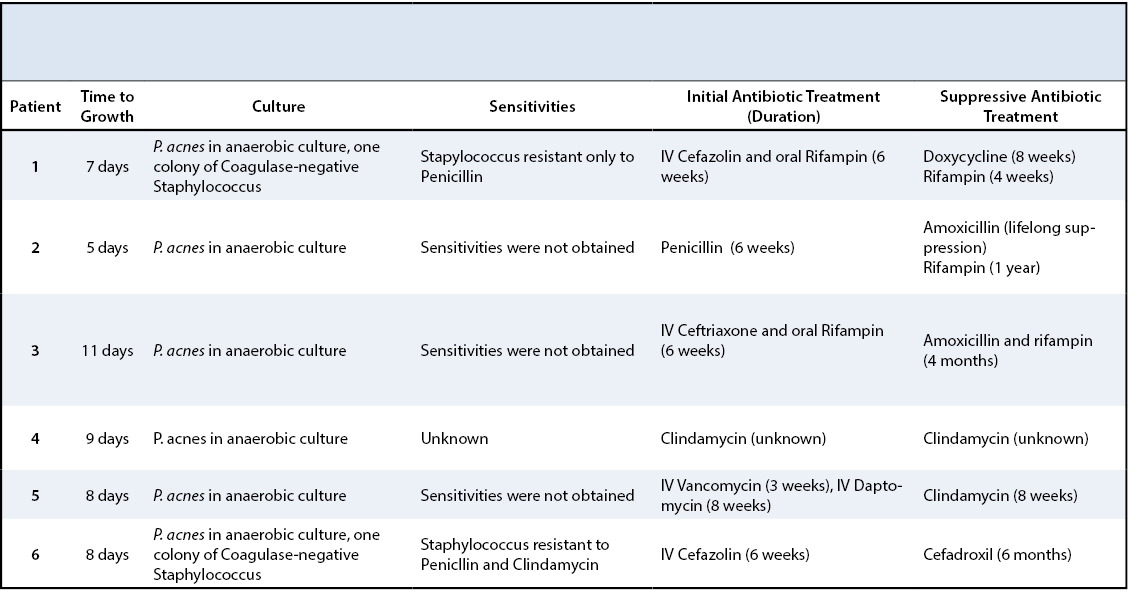
Two patients developed a symptomatic postoperative infection within 3 months following surgical treatment while the other four patients developed positive cultures at a later date obtained at the revision surgery (mean 23.6 months, range 6-71 months). In all, the primary causative agent was P. acnes. Coagulase negative staphylococcus was also found in two patients.
In two out of the four patients, P. acnes had been cultured during a second surgery prior to referral to our service. The organisms that grew on culture were initially interpreted as contaminants, and prior to revision surgery at our institution no antibiotic treatment was provided.
Antibiotic therapy after surgical debridement and revision consisted of six to eight weeks of an intravenous antibiotic regimen including cefazolin, penicillin, ceftriaxone, clindamycin, vancomycin or daptomycin for an average of 7 weeks (range 6-11 weeks). This was followed by an oral regimen with one agent (clindamycin, amoxicillin, or cefadroxil) or a combination of one of these drugs with rifampin. Oral antibiotics were continued for an average of 21 weeks (range 2 and 6 months; one individual was placed on life long antibiotic suppression). The parenteral antibiotics were tailored towards the sensitivities of the bacterium when available (Table 2).
A 52-year-old woman and avid triathlete sustained a closed, displaced distal clavicle fracture of her non-dominant limb. She initially underwent coraco-clavicular screw fixation with a 4.5 mm cannulated screw. Three weeks postoperatively, the screw was noted to have migrated superiorly. She returned to the operating room, where the fracture was internally fixed with a hook plate and screws. Two months later, radiographs suggested the fracture had united and the plate was removed due to hardware irritation. Follow-up radiographs at eight weeks following plate removal demonstrated a nonunion, and the patient was referred for reconstruction. A third operation was performed four months following hook plate removal using a dorsolateral plate with four locking screws in the distal piece in addition to a 2.4mm anterior plate with five screws along with 3 cm autogenous iliac crest bone graft. Cultures revealed one colony of Coagulase-negative staphylococcus and moderate P. acnes.
She was treated with intravenous cefazolin in combination with oral rifampin for a total of six weeks, followed by eight weeks of oral doxycycline.
At thirty-four months status post revision surgery, she reported 0/10 pain on VAS, and an improvement from 66 to 9 points on the short Disability Arm, Shoulder and Hand Score (DASH). Physical examination demonstrated full range of motion of her shoulder. The patient was able to return to her competitive athletic lifestyle (Figure 1).
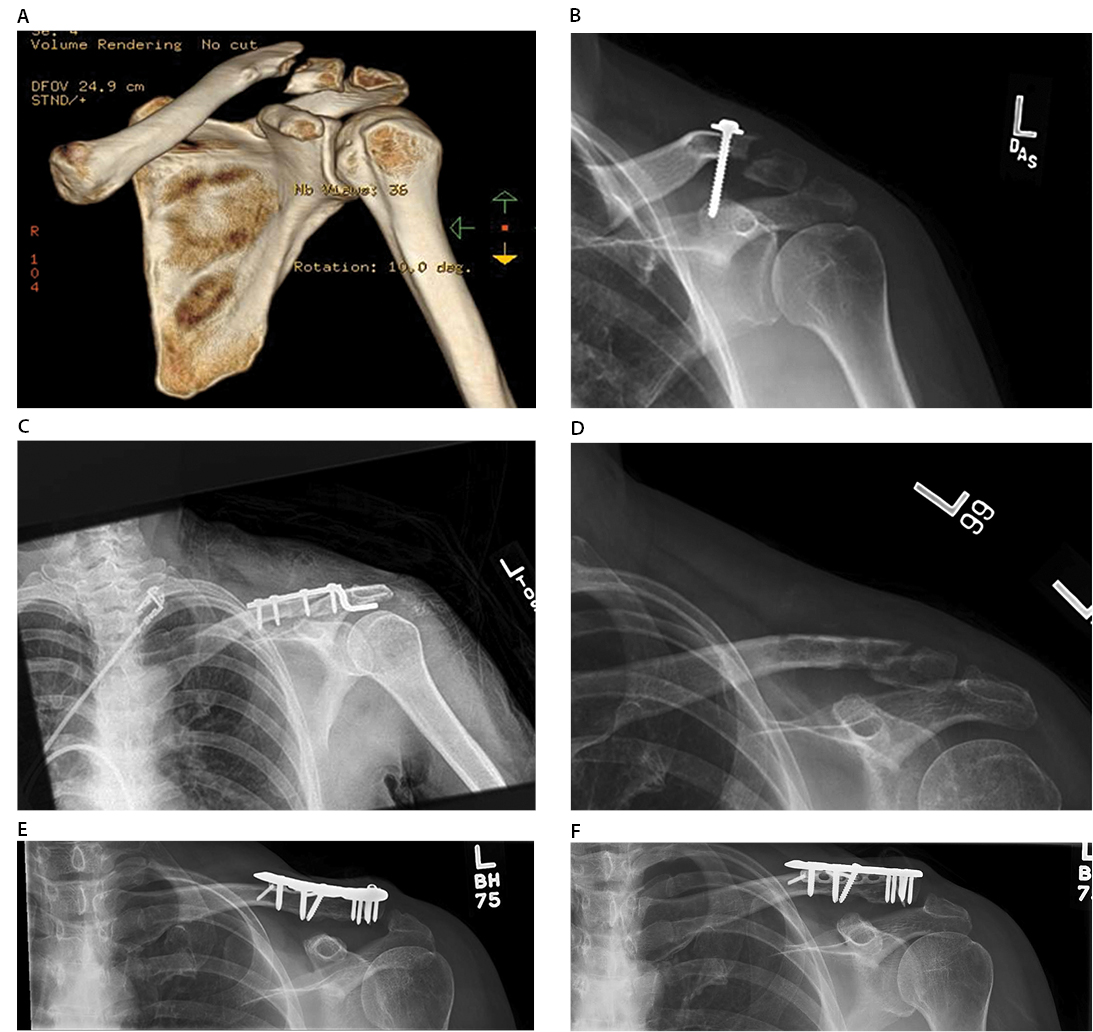
(A) Evidence of failure of fixation with a 4.5mm coraco-clavicular screw (B). Subsequent fixation with a hook plate and screws (C) and radiographs taken after removal of hardware demonstrating nonunion (D). Final clavicle radiographs (E/F) demonstrating healing of nonunion status post superior & anterior plating and screw fixation.
A 59-year-old male sustained a closed midshaft fracture of his right dominant clavicle from a fall. Surgery was performed at an outside institution with a plate and screws, which failed to heal. Two subsequent surgical attempts to achieve union with plate and screws and allograft bone graft followed.
A fourth attempt at our institution included autogenous iliac crest graft plus plate and screw fixation, which also proved to be unsuccessful. Intraoperative cultures demonstrated P. acnes, which was thought to be a contaminant due to multiple prior surgeries. The patient was referred to the senior author. Physical examination revealed a painful shoulder girdle motion with his pain scale on the VAS being 10/10 and DASH score of 95 points. The erythrocyte sedimentation rate was 16 mm/hr and C-reactive Protein 10.4 mg/L. Radiographs revealed an obvious non-union in addition to loose internal fixation.
Surgery was performed using a dual plate fixation including a 6-hole 2.7mm plate on the dorsal surface and 9- hole 3.5 mm on the anterior surface. A metatarsal allograft was used to bridge the defect at the nonunion site following debridement. Intraoperative cultures again revealed P. acnes. Parenteral penicillin was given for total of 8 weeks followed by oral amoxicillin and rifampin, which was anticipated to be lifelong. At three months post-op, radiographs demonstrated that his nonunion to have healed. At 43 months following his last revision surgery, his VAS score was 3/10, and his DASH improved from 95 to 61 points with full shoulder range of motion (Figure 2).
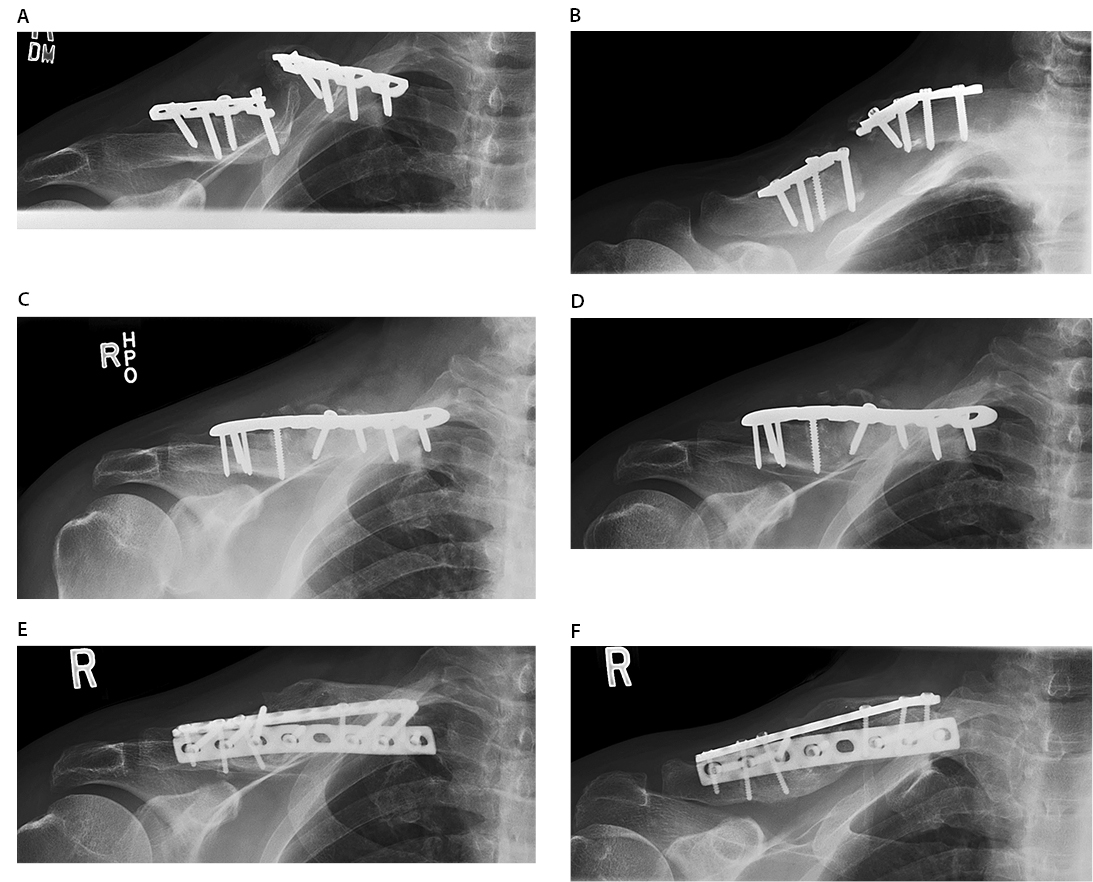
(A/B) Initial presentation demonstrating hardware breakage and nonunion of mid shaft clavicle fracture. (C/D) Radiographs demonstrating revision fixation of the clavicle fracture and nonunion. (E/F) Imaging of the re-revision fixation with double plating and screw fixation demonstrating healed nonunion.
A 21-year old college soccer player sustained a displaced midshaft clavicle fracture in her non-dominant extremity while playing soccer and underwent surgical fixation with a 3.5mm plate. Six weeks postoperatively, wound dehiscence occurred. Radiographs did not show any evidence of bony healing. She was taken to the operating room for irrigation and debridement of the surgical site. The plate was left in place. Cultures were obtained and grew P. acnes. Intravenous ceftriaxone in addition to rifampin was administered for six weeks followed by oral amoxicillin with rifampin. Four months status post irrigation and debridement, the plate was removed and revision internal fixation with double plating using a 5-hole 3.5mm anterior plate and 8-hole 3.5mm superior plate was performed. Cancellous bone grafting from the iliac crest was used to fill the 2cm gap from the apparent nonunion site. Cultures that were obtained at the revision operation remained without growth. Antibiotics were discontinued when bony union was evident on CT scan four months after the revision procedure. At five months following her revision surgery, the patient report 0/10 on VAS with a DASH score of 2 and returned to playing soccer.
After eradicating the infectious organism, all six patients demonstrated healing of the infected nonunion on follow-up radiographs.
All six patients improved in regards to their Quick DASH Score, functional motion, and pain scale when the treatment was completed. The DASH Score improved from 54±32 (n=5) to 22±72 (n=5) points at final follow-up (25±19 months, range 3- 43months). The range of motion (n=5) of the affected shoulder postoperatively demonstrated on average abduction of 160±35 degrees, forward flexion of 153±46 degrees, external rotation of 75± 26 degrees and VAS pain scale decreased from 4.8±3.1 to 1±1.7 (Table 3).
Overall, two patients underwent four procedures, three patients underwent three operations and one patient underwent two operations to achieve healing of their infected non-unions. All patients demonstrated union at final follow-up. Evidence of bony healing following revision surgery was apparent in less than 3 months in all patients (8± 3 weeks, range 4-12 weeks).
Complications included an initial cortical screw backing out slightly in one patient, which remained mildly symptomatic but did not interfere with functional activities. Two patients had allergic reactions to the antibiotic therapy. Upon change of the antibiotic, the symptoms subsided.
Infection after surgery about the shoulder girdle is an uncommon condition but can have devastating impact on the shoulder function.17 P. acnes was once thought to be a contaminant but now is recognized as one of the most common and important pathogens causing infection after surgical procedures about the shoulder girdle.10, 16, 20 With the increase in operative treatment of clavicle fractures, there is a potential for an increase in surgical complications such as infections.
Duncan et al.6 were the first to report on P. acnes infection after surgical treatment of the clavicle. In their series of six patients, three patients were found to have P. acnes inoculation. All three patients were noted to have pain even after eradication of the infection. Liu et al.11 reported on seven patients with clavicle fracture who developed postoperative infection, although none were caused by P. acnes.
P. acnes is a gram-positive anaerobic bacillus that is found on the skin, especially in sebum excreting sebaceous follicles. It was first noted to be the source of infection in shoulder surgery in 1999,19 with an increasing incidence reported in subsequent studies.2, 7 The explanation for why the shoulder appears to be the most commonly affected area after surgical intervention by this bacterium remains not fully understood. The shoulder area has the highest density of sebaceous glands and most lipophilic skin, which may be a predisposing factor. P. acnes is notorious for having slow growth in a culture medium (requiring a minimum of 6 days) and can be difficult to detect.
Lutz et al. found that it took an average of 11 days for this bacteria to grow from specimens associated with arthroplasty and osteosynthesis infections. In their study, early infections resulted in a slightly shorter duration until cultures were positive in comparison to late infections. (8.4 and 13.5 days, respectively)12 It should be noted that ESR and CRP concentration are insensitive indicators for Propionibacterium osteosynthetic shoulder infection. It is rare for P. acnes to present itself with a sinus tract communicating with the osteosynthetic material and similarly rare to demonstrate visible purulence at the implant site. However, it is prudent to have a high suspicion for infection, in particular P. acnes, in chronic nonunion after surgically reconstructed clavicle fractures. It is advisable to obtain at least three samples of anaerobic cultures, which should be held for at least 14 days to increase the diagnostic value of detecting the pathogen.1, 4, 9, 18 Asseray et al.1 determined different criteria to improve the probability of diagnosing infection. They found that a probability of >90% was achieved if at least two positive deep cultures were present with one of the following criteria: intraoperative signs of infection, the presence of an orthopaedic implant or revision surgery. If only one positive deep culture was present, the diagnosis of P. acnes required three of the following criteria: local signs of infections, inflammatory biological markers, orthopaedic device and revision surgery to achieve >90% probability of an actual P. acnes infection.
Osmon et al.15 published guidelines on the treatment of prosthetic joint infection and recommended parenteral penicillin or ceftriaxone for P. acnes infection. The optimal choice of antibiotic medication, however, has not been established due to the paucity of the data for osteosynthetic infections with P. acnes. Thus, a few authors have used a variety of antibiotics such clindamycin, vancomycin, cephalosporins or linezolid. Rifampin appears to offer synergy in the eradication of P. acnes biofilms,2, 5, 7 though the role of this antibiotic in treatment is not clear yet due to the paucity of the available data, and drug interactions complicate its use. Rifampin should only be used in combination with another antibiotic, as it is thought to aid in antibiotic penetration into the bone architecture. Due to the limited number of patients in this series we are not able to give general recommendations on the antibiotic treatment therapy.
Currently there is no treatment algorithm for managing P. acnes infection of clavicular nonunion. Controlled clinical research is necessary to identify the optimal antimicrobial approach to these infections. Two general approaches appear feasible for chronic nonunions (>3 months post-op), which can be amenable to either single-stage revision plating versus two-stage revision including irrigation and debridement and revision fixation.8 This decision should be made on an individualized basis. Based upon the senior author’s experience, we suggest a staged procedure if there is suspicion for chronic infection or massive bone loss in comparison to chronic infection with mild to moderate bone loss. Double plating with intercalary bone graft either from the iliac crest or allograft may be required to provide the stability to counteract the inherent rotational forces across the clavicle. Parenteral antibiotics should be started as soon as the pathogen is identified. Acute infection (<3 months post-op) should be treated either with local irrigation and debridement with retaining hardware until union is observed with subsequent removal of hardware or revision fixation with plate and screw fixation. It is advisable to keep three samples of cultures obtained during a revision procedure for at least 2 weeks if there is suspicion for P. acnes infection.
This is the first series of P. acnes infection after clavicle fracture ORIF. It is difficult to diagnose and when unrecognized can result in significant long-term impairment of the patient. It is necessary to have high suspicion of infection in clavicle nonunion after surgical fixation. No clinical guidelines currently exist. Single stage or two stage procedures in combination with long-term parenteral antibiotic therapy may lead to union and good outcomes.