Retained Knife Blade in the Popliteal Fossa: A Case Report and Review of the Literature
Timilehin O. Wusu, MD, Natalie Casemyr, MD, Mostafa Abousayed, MD, Malcolm R. Smith, MD, John Y. Kwon, MD
Disclosure Information©2015 by The Orthopaedic Journal at Harvard Medical School
We present a case of a 63-year-old male who presented with a retained knife blade in the popliteal fossa. Patient presented after an assault complaining of left knee pain and inability to flex his knee. He had a 3cm transverse entry wound in the anteromedial aspect of his left knee. His sensory motor exam of the left lower extremity remained completely intact. Vascular exam only notable for slightly diminished dorsalis pedis pulse compared to the contralateral side. His straight leg raise was intact, with knee stable to varus/valgus and Lachman stress testing. AP/Lateral radiographs demonstrated a 3x12 cm retained knife blade in the popliteal fossa. The patient was placed in a knee immobilizer and taken to surgery where the blade was extracted from a medial incision along the junction of the vastus medialis and sartorius. Amazingly, intraoperative exploration of the wound demonstrated only one significant intraarticular injury, traumatic laceration of the anterior horn of the medial meniscus, which was repaired. No vascular injury was identified. The remainder of the postoperative and rehabilitative course was uneventful.
This is an unusual case of a retained knife blade in the popliteal fossa from an anterior entry wound without vascular nor ligamentous injury. The retained knife blade is a seldom-reported injury with the majority of cases involving the head, neck and thoracic regions. ATLS protocols should be followed for any patient with penetrating injury with focus on initial stabilization and resuscitation. Simple withdrawal of penetrating object in the ED should only be performed if potential for life and limb-threatening vascular injuries can be excluded. Otherwise extractions should be performed in the operating theatre with appropriate consultation of other surgical specialties.
We present a case of a 63 year old male who presented with a retained knife blade in the popliteal fossa. We discuss management and present a review of the literature.
The patient is a 63 year old man who presented to an emergency department with a stab injury to the left knee and blunt facial trauma. He reported being assaulted at home by an unknown assailant but was a poor historian and unable to provide other details. He was initially evaluated at an outside institution where a primary survey was performed with clearance of head, cervical spine and facial injuries via multiple CT scans. He was subsequently transferred to our institution for further care.
Upon presentation, vital signs were within normal limits, and he complained of face and left knee pain with inability to flex his knee. He denied tingling or numbness and had no difficulty moving his foot or ankle distally. His past medical history was significant for hepatitis C, liver cirrhosis, post traumatic stress disorder, bipolar disorder and polysubstance abuse with multiple prior evaluations for assault-related trauma and alcohol intoxication.
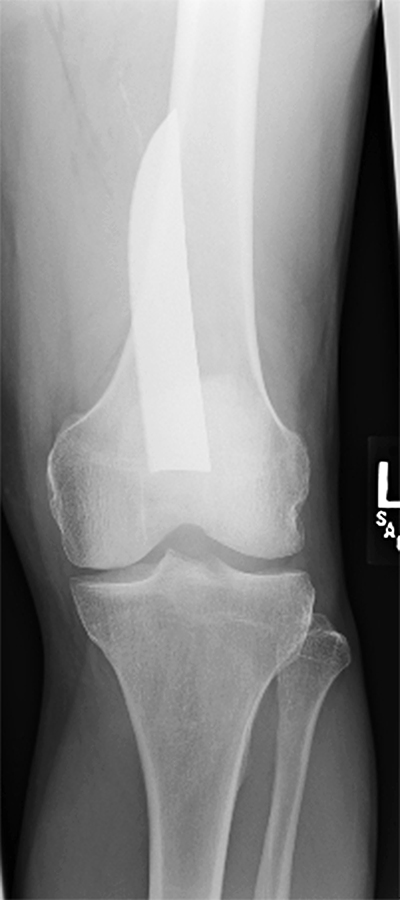
Physical examination revealed right periorbital ecchymosis in an otherwise oriented patient. There was a 3 cm transverse entry wound along the anteromedial aspect of his left knee just distal to the patella with an associated mild effusion and mild sero-sanguinous drainage (Figure 1). No additional wounds were found. Limited examination of the left knee revealed a palpable patellar tendon with intact straight leg raise, and negative Lachman test with no varus/valgus instability. He was unable to flex the knee due to pain. Distal motor sensory exam of the left lower extremity was fully intact. Vascular exam was notable for a slightly diminished left dorsalis pedis pulse compared to the contralateral side. Posterior tibial pulses were full and symmetric. The popliteal fossa was soft and compressible without palpable thrill.

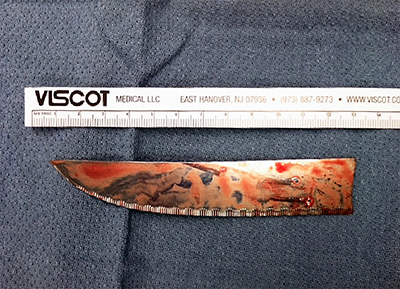
Laboratory results were within normal limits but urine toxicology was positive for cocaine, ethanol and benzodiazepines. Ankle-brachial indices were normal and symmetric. Pulse volume recordings were triphasic, pulsatile and symmetric. Plain x-rays of the knee revealed a retained knife blade lying along the posterior aspect of the femur (Figure 2 and Figure 3).
The patient was initially placed in a knee immobilizer and admitted to the Orthopedic Surgery Service. Tetanus was updated and IV antibiotics were administered. The Vascular Surgery Service was consulted and no further imaging studies were recommended. Analgesics and DVT prophylaxis were started. Psychiatric consultation was obtained to help manage his polysubstance abuse.
Surgical exploration of the wound was performed by the senior authors with exploration of the popliteal vessels first. A tourniquet was placed but not inflated. The leg was prepped and draped in standard fashion with the patient in supine position. A long medial incision was made along the junction of the vastus medialis and sartorius. The vastus medialis was retracted superiorly and the hamstring complex was retracted inferiorly. The popliteal vein and artery were clearly identified and were found to be grossly normal without active extravasation. Deep retractors were placed and the knife blade was then visualized immediately deep to the vessels on the posterior aspect of the femur with the sharp edge facing the vessels. The knee was flexed to relax tension, allowing the vessels to be adequately mobilized and carefully retracted. The blade was extracted uneventfully (Figure 4). The vessels were then fully dissected along their visible length with no evidence of adventitial injury. The pulse was palpable without thrill. Intraoperative pulse volume recordings had good wave forms. The vascular surgery team then explored the vascular structures and no vascular injury was indentified.
The knee joint was further assessed with proximal and distal extension of the transverse entry wound and careful inspection of the intraarticular structures. The anterior cruciate ligament was intact. There was a traumatic laceration of the anterior horn of the medial meniscus and a small chondral shaving off the distal femoral condyle with no exposed subchondral bone. No other intraarcticular injury was identified. The joint was thoroughly irrigated and the anterior horn of the medial meniscus then repaired. A layered closure over a drain left in the popliteal fossa was performed. The knee was reexamined and found to be ligamentously stable.
Postoperatively, the patient continued on perioperative antibiotics with close observation of the wound for early signs of infection. The drain was removed on postoperative day two. He remained neurovascularly intact in the left lower extremity with normal vital signs. The patient was discharged with a knee brace on postoperative day three. He was seen 2 weeks later at the outpatient clinic where he denied focal and general symptoms and had excellent mobilization of the knee without difficulty. His wound was satisfactory with no sign of infection and sutures were removed. The remainder of his postoperative and rehabilitative course was unremarkable.
We report an unusual case of a retained knife blade in the popliteal fossa from an anterior entry wound without neurovascular or ligamentous injury. We believe the knife entered through the anteromedial wound with the knee flexed, as if in a seated position. The patient then likely extended his knee, as if to arise to fend off his assailant, with consequent breakage of the blade.
The retained knife blade is a rarely reported injury with the majority of case reports and small case series involving injuries to the head, maxillofacial, neck and thoracic regions.1-5 Patients with penetrating trauma should be managed according to ATLS guidelines, with focus on initial stabilization and resuscitation. All patients with penetrating injuries must be evaluated for tetanus prophylaxis and antibiotics may be considered. Providers must maintain a high suspicion for retained blades if the wound is more than superficial and the entire knife is not recovered.
Patients in hemodynamic shock should be taken for emergent surgical exploration and intervention, as should patients with pulsatile hemorrhage, bruit, absent distal pulses or expanding hematomas.4, 6 Hemodynamically stable patients warrant further diagnostic studies.4 Simple withdrawal of the penetrating object may be performed in the emergency room if the potential for life and limb-threatening vascular and visceral injuries can be excluded. More involved extractions should be performed in the operating theatre with appropriate consultation from other surgical services.4 Patients with retained blades and associated major vascular/solid organ injuries may be hemodynamically stable upon presentation as the retained implement can act as a tamponade.4 In a series of 154 stab wounds reported by Hanoch et al,4 patients went on to hemodynamic collapse after unplanned extraction of a retained knife by the victim or inexperienced medical personnel.7
Sobnach et al. reviewed 33 patients who presented with retained knife blades from 1996-2007. Most of the retained blades were in the thorax (40%) and neck/back region (21%), with fewer in the extremities (12%) and abdomen (3%). They recommend a low threshold to evaluate for infection, especially in cases of retained thoracic blades, which were significantly associated with post-operative sepsis.4 Most authors addressing extraction of retained blades recommend exploration and removal through the tract of the entrance wound itself.2, 4, 8 In the case presented here, the anterior entrance wound was not conducive for extraction of the retained blade in the popliteal fossa as the blade could not be removed under direct visualization nor the neurovascular bundle directly assessed. Because of the concern for possible associated vascular injury, a medial approach was used to better allow for further exposure and control of the vessels proximally and distally if needed.
Stab wounds to the knee are associated with a wide spectrum of injuries and necessitate careful assessment for proper diagnosis. Penetrating injuries to anterior knee can result in partial or complete quadriceps or patellar tendon laceration, and may require advanced imaging to confirm diagnosis. Management of acute tendon injuries can be challenging and although primary repair is often the treatment of choice, late reconstruction may sometimes be required.9 Deeper wounds penetrating the joint capsule place intraarticular structures at risk. As pain often limits adequate examination, exam under anesthesia is often performed to help identify possible internal derangement. Traumatic meniscal injuries are usually addressed at the time of initial surgical exploration. Treatment follows the general guidelines for meniscal injury management with tears in the red-red or red-white zones typically amenable to repair and other injuries often treated with partial meniscectomy.21-25 The ideal timing for management of associated ligamentous knee injuries is not as clear cut. While ligamentous injury can be addressed at the time of initial surgical exploration, it is more commonly delayed with most advocating treatment within 2-4 weeks of injury.10, 11, 12 Serious associated injuries, such as vascular injury necessitating repair, may prohibit management of ligamentous injuries in the early period.13-19 In rare cases of multi-ligamentous injuries with instability, an external fixator can be placed for a period of 2-6 weeks prior to pursuing definitive management.20
Intraarticular penetrating knee injuries may also result in osteochondral lesions, which represent a long standing challenge to orthopaedic surgeons.26 Management strategies include repair with reduction and fixation of the osteochondral fragment, reconstruction with techniques to induce fibrocartilage formation or defect management with autograft and allograft constructs, and finally replacement in the setting of progression to advanced osteoarthritis.27
Penetrating injuries involving the popliteal fossa are at high risk for concomitant nerve or vascular injuries. Nerves may be injured directly by the sharp object or secondarily due to ischemic neuropathy from vascular compromise or compression neuropathy from an expanding hematoma or subsequent pseudoaneurysm formation. The common peroneal nerve is the most frequently injured nerve with rare cases of tibial nerve injuries reported.28 Injuries to the common peroneal nerve classically present with a foot drop and are difficult to treat with relatively poor prognosis. Electromyogram and nerve conduction velocity studies may be obtained to help guide treatment. Conservative treatment consists of physical therapy and bracing. Surgical exploration with neurolysis or repair and/or grafting is attempted only if conservative measures fail or in rare cases where primary surgical exploration is justified.29, 30, 31
Vascular injury is present in 2% of traumatic knee injuries.32 The evaluation of patients with penetrating extremity trauma in close proximity to major vascular structures with advanced studies such as angiography and CT angiography remains controversial. While angiography has traditionally been considered the gold standard, more are advocating for the use of noninvasive methods such as duplex ultrasonography.4, 33 After an extended review of 514 penetrating extremity injuries with 60 stab wounds and 454 gunshot wounds, Anderson et al. recommend angiography for gunshot wounds in high risk areas and suggested that clinical evaluation alone may be sufficient for stab wounds to the extremities. If further evaluation for occult vascular injury is pursued, they suggest that ultrasound is the screening test of choice.6, 34 While Anderson et al. reported no occult vascular injury in stab wounds to the extremities, Turcotte et al’s assessment of the use of angiography in traumatic vascular injuries to the extremities found that occult injuries are not uncommon and vascular exam may be normal distal to the lesion in 25% of cases.35 As an end artery with associated poor collateral circulation, injuries of the popliteal artery have been correlated with poor prognoses which result in loss of limb. Penetrating injuries in close proximity to the popliteal vessels should be viewed carefully. Soft signs of vascular injuries including hematomas, neurological deficit or bruits can sometimes be present and thus provide clues to possible vascular injury and hence the need for further diagnostic measures.
Popliteal artery aneurysms have been reported as late sequelae of popliteal vessel injury. They have been described more frequently in military injuries but rare similar cases have been reported in civilian practice following blunt and penetrating trauma. They generally form as a result of disruption of the vessel wall with consequent hematoma formation, which is contained by the surrounding structures leading to fibrous pseudocapsule formation and often knee flexion contracture.36, 38 The severity of arterial wall injury determines the time interval at which the pseudoaneurysm is formed which may vary from hours to years. Rich et al. estimated that almost half of the pseudoaneurysms became clinically evident after 30 days.37 In their retrospective review of cases from 1998-2000, Woogler et al. reported seven cases of popliteal pseudoaneurysms with an average of one month delay in presentation (range 1-24).38
Penetrating injuries to the extremities are often serious and can be limb or life-threatening. Retained foreign bodies require a high index of suspicion for associated injury. Careful assessment is mandatory for adequate management. While the study of choice for diagnosing vascular injuries is still debatable, most are advocating the use of non-invasive studies, such as duplex ultrasonography, if clinical examination is not sufficient. Extraction is typically performed in the operating room, particularly if hemodynamic instability is anticipated or associated injuries requiring surgical intervention are present.