Occupational Sharps Exposures Among Orthopaedic Surgery Residents: A Multi-institutional Survey Study
Dafang Zhang, MD, Ehsan Saadat, MD, George S. M. Dyer, MD, Mitchel B. Harris, MD
The authors report no conflict of interest related to this work.
©2015 by The Orthopaedic Journal at Harvard Medical School
BACKGROUND Sharps exposures are an occupational health hazard to health care professionals and increasing among surgeons. Surgeons in training are particularly at risk, but injuries are not always reported. The objective of this study is to measure the prevalence and reporting of occupational sharps exposures among orthopaedic residents, to understand how these injuries occur, and how residents decide whether or not to report them.
METHODS A cross-sectional study was performed using a survey questionnaire distributed to 61 residents in an ACGME accredited orthopaedic surgery residency program at a single time point. The survey asked respondents their year in training, details about their experiences with sharps exposures, and details about the reporting of these exposures.
RESULTS 90% (55 / 61) of residents completed the survey questionnaire. 69% of residents identified at least one sharp exposure during their residency training. The likelihood of having at least one sharp exposure increased with year in training, while the number of sharps exposures within any given year decreased with year in training. 76% of residents with a sharp exposure have utilized occupational health, while 42% have failed to report a sharp exposure. 90% of residents who reported an exposure followed through with occupational health recommendations.
CONCLUSION Orthopaedic surgery residents are particularly susceptible to occupational sharps exposures, especially early in their training. Safety training should focus on junior trainees. All staff, particularly this group, should be encouraged to report injuries.
Accidental sharps exposures are an occupational hazard of health care professionals. The incidence of occupational sharps exposures, defined as a percutaneous injury with any object penetrating the skin, is estimated to be between 14 to 839 injuries per 1,000 health care professionals per year.1 Sharps exposures carry a significant risk of transmission of blood-borne pathogens, including hepatitis B,2 hepatitis C,3 and HIV,4 both to the provider and to the patient. The economic burden of a sharp exposure can be as high as nearly $4,000 per percutaneous injury.1 Finally, sharps exposures are a source of anxiety and emotional distress to health care professionals who sustain them.
Among health care professionals, surgeons are at unique risk for occupational sharps exposures.5, 6 Orthopaedic surgeons use a wide array of sharp instrumentation and routinely handle sharp bone edges; as a result, they are at unique risk of percutaneous injuries during surgical procedures.7, 8 Surgical residents in training are especially vulnerable to sharps injuries.5, 7, 9 Moreover, when sharps exposures occur, a large percentage are never reported to the appropriate occupational health department,10 posing a health hazard to the surgeon and patient.
The objective of this study is (1) to measure the prevalence of occupational sharps exposures among orthopaedic surgery residents at a single, multi-institutional residency program, (2) to measure the rates of reporting of occupational sharps exposures among orthopaedic residents, and (3) to understand how these injuries occur and how residents decide whether or not to report them. We hypothesize that sharps exposures are highly prevalent among orthopaedic residents, but that the minority of injuries are reported. With our understanding, we hope to formulate strategies for safer practices for orthopaedic surgeons in training.
After Institutional Review Board review and exemption, a survey questionnaire regarding the incidence and reporting of sharps exposures was distributed to 61 residents within an Accreditation Council for Graduate Medical Education (ACGME) accredited orthopaedic surgery residency program. All residents within the program completed the survey except for the two co-investigators of this study. Since the residency program is among the largest orthopaedics programs in the U.S., and its residents train at four tertiary care centers, it was taken to be an appropriate study population. Residents were asked to complete either a hardcopy or an equivalent online version of the questionnaire on a voluntary, anonymous basis.
The questionnaire asked respondents to identify their post-graduate year in training, whether or not they have sustained an occupational sharps exposure, and if so, how many. Choices included 1, 2, 3, 4, 5, greater than 5, and greater than 10 exposures. Those reporting an exposure were asked the post-graduate year in training when it occurred, the type of sharp (suture, scalpel, hollow-bore needle, bone fragment, surgical instrument, etc.) that caused the injury, and the type of procedure (trauma, joints, hand, etc.) in which the injury occurred. Multiple choices were allowed. The questionnaire further asked whether the exposure was reported to occupational health. If so, respondents were asked to identify reasons why they did so, and if not, respondents were asked to identify reasons why they did not. Choices for reasons for reporting the exposure included personal health, hospital policy, supervisor instruction, or other. Choices for reasons for not reporting the exposure included perceived insignificant exposure, perceived low risk patient, being too busy, not knowing the responsibility to report, not knowing the location of occupational health, the inconvenience of the location of occupational health, or other. Multiple choices were allowed. If the respondent reported an exposure to occupational health, the questionnaire asked whether they followed through with occupational health recommendations. If not, respondents were asked to identify reasons why they did not. Choices for reasons for not following occupational health recommendations included perceived insignificant exposure, perceived low risk patient, being too busy, concerns about medication side effects, and other. Multiple choices were allowed.
Responses were tabulated and analyzed by post-graduate year, number of sharps exposures per resident, type of sharp, and type of procedure. Sharps exposures per type of procedure were further adjusted for the amount of time residents spend on each particular rotation. Descriptive statistics were calculated for the incidence of sharps exposures where appropriate. Fisher’s exact test was performed for comparisons of sharps exposures between each post-graduate year and the mean. Spearman’s rank correlation coefficient was used to determine the correlation between sharps exposures and post-graduate year. The standard significance criterion of α=0.05 was employed for all statistical tests.
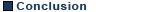
The survey questionnaire was completed by 90% (55 / 61) of residents. Of those who completed the questionnaire, 69% (38 / 55) identified at least one sharp exposure during their residency training, although some residents identified many more (Figure 1). The median number of sharps exposures among residents was 1. Two residents reported more than 10 sharps exposures during residency.
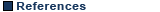
The number of residents who have had at least one sharp exposure during residency increased with each post-graduate year. The number of residents with a history of at least one sharp exposure can be modeled as a polynomial function of post-graduate year (Figure 2). Fisher’s exact tests showed that PGY5 residents were comparatively more likely to have ever sustained a sharps injury than the cohort population (p-value = 0.01). The occurrence of sharps injuries, however, decreased with each post-graduate year, with PGY1 residents being most at risk (ρ = -1.00, p < 0.001). The number of sharps exposures per year decreased as a function of post-graduate year (Figure 2). In other words, lifetime prevalence of sharps exposures increased with increasing post-graduate year, but incidence decreased.
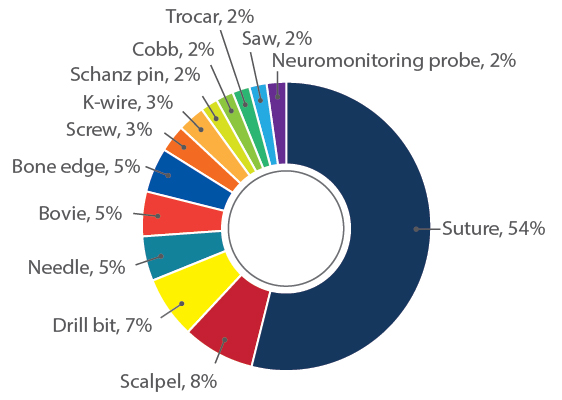
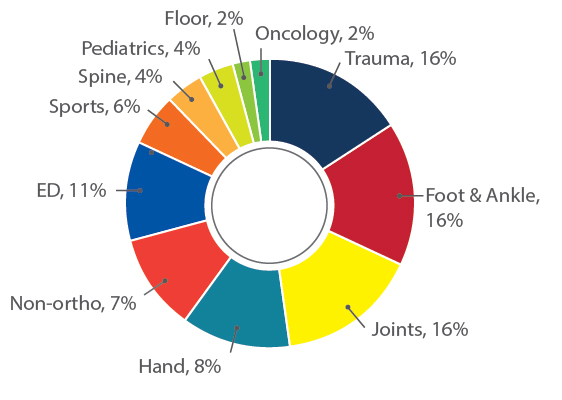
Thirteen types of sharps were identified to cause sharps injuries among residents; however, the majority (54%) of sharps injuries were caused by suture needles (Figure 3). Eleven unique types of procedures were identified to cause sharps injuries among residents. This data was normalized for the amount of time residents spent on each particular rotation (Figure 4). The most common procedure in which a sharp exposure was sustained was an orthopaedic trauma procedure in the OR. The two least common procedures in which sharps exposures were sustained were an orthopaedic oncology procedure in the OR and a floor procedure.
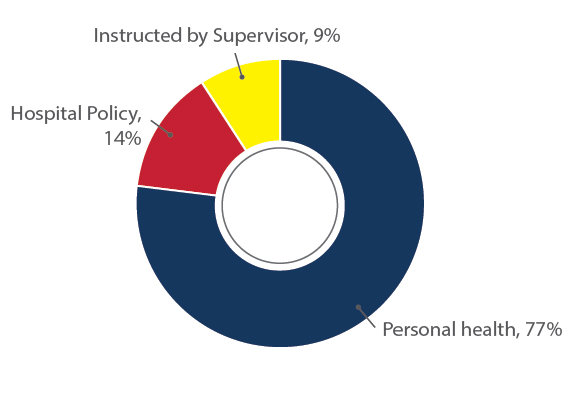
Of the residents who have had a sharp exposure during their residency, 76% (29 / 38) have reported at least one sharp exposure to occupational health, whereas 42% (16 / 38) have not reported at least one sharp exposure to occupational health. 77% of residents who reported identified concern for personal health, 14% of residents identified hospital policy, and 9% of residents identified supervisor instruction as the reason for reporting sharps exposures to occupational health (Figure 5). 50% of residents identified perceived insignificant exposure, 31% of residents identified perceived low risk patient, 13% of residents identified being too busy, and 6% of residents identified the inconvenience of the occupational health location as the reason for not reporting sharps exposures to occupational health (Figure 6). Of the residents who reported a sharp exposure to occupational health, 90% (26 / 29) followed through with occupational health recommendations. Of the four residents who did not follow through with occupational health recommendations, two did so because of a “perceived low-risk patient,” one did so because of a “perceived low-risk patient,” and one did so because he or she was “too busy.”
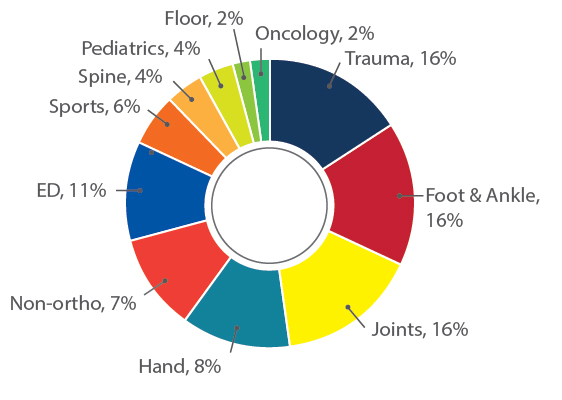
Sharps exposures are an occupational health hazard to surgeons. Despite the introduction of safety syringes and anti-needlestick devices,11 the incidence of sharps injuries continues to increase in the surgical setting.12 Recent studies have suggested surgical trainees may be a particularly vulnerable population to sharps injuries.5, 7, 9 In the present study, we have found that 69% of our orthopaedic residents have been injured by sharps at work. The number of sharps exposures per resident varied widely in this study. The reasons for this variance are unknown, but may include inherent dexterity, adherence to safe practices, differing degrees of surgical oversight, or fatigue level at the time of injury. The risk to residents of having had an occupational sharp exposure increased as a polynomial functional of post-graduate year. However, although the lifetime prevalence of sharps exposures increased with increasing post-graduate year, the incidence decreased with each additional year in training. In accordance with prior studies, sutures needles were responsible for the majority of sharps injuries.7, 9 Orthopaedic trauma OR procedures were most often associated with sharps exposures.
The incidence of sharp exposures was found to be highest in the intern year of training. This finding is supported by prior studies9, 10 and partly explained by the fact that a cohort of residents in progressive post-graduate years were surveyed and residents could only have sustained sharps exposures in training years they have already completed. However, recent studies have raised concerns that interns are particularly vulnerable to occupational sharps injuries and feel unprepared to perform common procedures when they begin internship.13, 14 Some orthopaedic residency programs, including ours, have implemented dedicated surgical skills training programs for interns outside of normal clinical duties.15-17 These provide both didactic exposure to orthopaedic surgery as well as practical exposure to orthopaedic techniques. Critical analysis of these surgical “boot camps” across multiple specialties, including general surgery, orthopaedic surgery, and neurosurgery, have found comparable resultant improvements in interns’ technical skills, non-technical skills, and knowledge.18 Surgical skills training curriculums emphasizing high-fidelity simulation and directed feedback may be a feasible means of moving towards a safer work environment for both patients and surgeons.
Underreporting of sharps exposures is a recognized problem. Approximately one-third of sharps exposures are unreported.9,10 In the present study, we found that 76% of orthopaedic residents reported a sharp exposure to the occupational health department appropriately; however, 42% of residents had at least one unreported sharp exposure. Residents were predominantly motivated to report exposures by concern over compromise to personal health. When exposures were not reported, a number of rationales were identified, including a belief that the exposure was insignificant, a perception that the patient was “low-risk,” being too busy, and the occupational health department being inconveniently located. When exposures were reported, occupational health recommendations were followed 90% of the time. Since a high adherence rate was found to occupational health recommendations, future focus should be towards increasing residents’ rates of reporting sharps exposures. Underreporting may represent a need for resident education on sharps exposures or a need for a more convenient reporting process, and future studies should aim to distinguish between these two.
One limitation of our study is that the study sample consisted of residents of a single residency program. However, measures of safety at the four member hospitals of this combined program are similar to reported national norms. A second limitation of our study is that survey responses were collected at a single time point, approximately 3 months into the academic year. Residents of each post-graduate year would be expected to have more sharps exposures by the end of the academic year. A final limitation of our study is the potential for information bias. Since we asked respondents to recall a past event, their responses are susceptible to factual inaccuracies of memory. Residents who have had a sharp exposure may also be less likely to admit it than residents who have not, although this form of response bias is mitigated by the anonymous nature of the survey.
Occupational sharps exposures are an important health hazard to orthopaedic surgeons. Orthopaedic surgery residents are particularly susceptible to occupational sharps exposures, especially early in their training. Efforts to decrease sharps exposures in junior surgical trainees is likely to have a positive impact on the health and emotional well-being of surgeons in training, to reduce health care costs related to the treatment of sharps exposures, and to improve patient care. Training for injury prevention should focus on junior trainees. Residents who report sharps exposures to occupational health have a high likelihood of following through with occupational health recommendations. Rates of reporting of sharps exposures may increase if more convenient and streamline processes for occupational health reporting were implemented.