Is Distal Fixation Necessary in Cephalomedullary Fixation of Pertrochanteric Femur Fractures?
Factors Associated with Blade Cut-Out
Dan Tobert, MD, Steve Huffaker, MD, PhD, Mitchel B. Harris, MD
The authors report no conflict of interest related to this work.
©2015 by The Orthopaedic Journal at Harvard Medical School
INTRODUCTION Failure of fixation after femoral cephalomedullary nailing for pertrochanteric (PT) femur fractures is a major source of morbidity and mortality in the elderly population. Several studies have looked at patient demographics and technical factors of fixation as predictors for blade cut-out, however, none have examined the effect of distal locking screw placement or other factors such as reamed versus unreamed CMN placement. We sought to investigate the role of distal fixation in blade cut-out and implant failure.
METHODS Patients who underwent initial surgical fixation of a pertrochanteric femur fracture with a long cephalomedullary nail device and subsequently had revision or conversion surgery of the original implant were included in the study. Demographics were extracted from the medical record and all operative notes were evaluated for documentation of femoral canal reaming during the initial fracture fixation as well as any notable aberrancies of the case. The primary outcome was revision for blade cut-out.
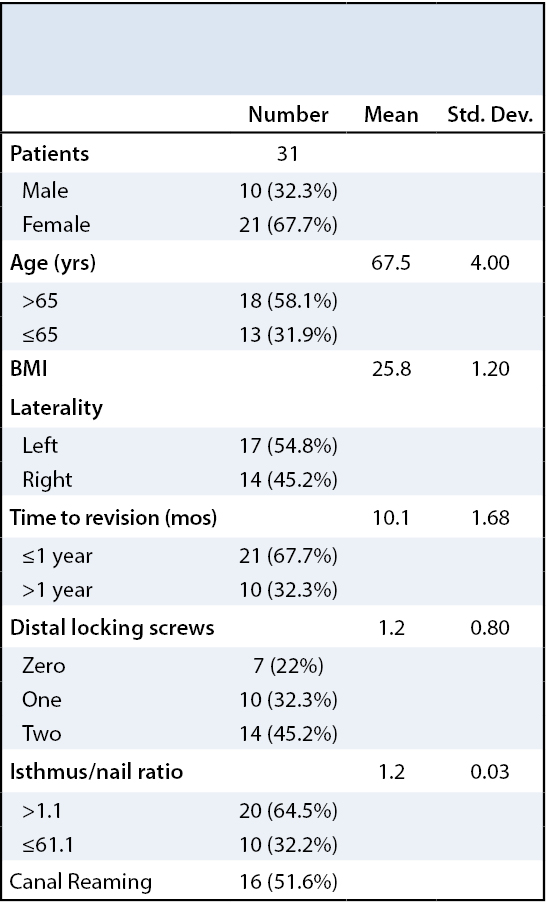
RESULTS Thirty-one (31) patients met the inclusion criteria for this study. Age >65, time to revision, an isthmus/nail ratio of >1.1 and unreamed canals were found to be associated with revision for blade cut-out. There was not a significant association between gender and the number of distal locking screws.
CONCLUSION Patients undergoing revision for blade cut-out were significantly more likely to be>65 years old, have initially undergone unreamed nailing, have a larger isthmus/nail ratio and be revised within one year. We did not find an association with revision for blade cut-out and distal locking screws. However, we argue and demonstrate from a small sample set that the effective working length of the CMN, namely whether isthmic purchase is present, is also an important consideration during the treatment of these fractures.
Failure of fixation after femoral cephalomedullary nailing for pertrochanteric (PT) femur fractures is a major source of morbidity and mortality in the elderly population.1 Blade cut-out (Figure 1) has been recognized as a prevalent type of catastrophic failure.2 Several studies have looked at patient demographics and technical factors associated with fixation as predictors for blade cut-out,3,4 however, none have examined the effect of distal locking screw placement or the fit of the implant within the femoral canal. There is currently no consensus regarding the value of distal locking screws with long cephalomedullary nails (CMN) in the treatment of PT femur fractures. Our aim was to identify factors associated with blade cut-out and implant failure aside from proximal fixation placement (TAD) when treating PT fractures with CMN. Specifically, we sought to identify the incidence of blade cut-out and implant failure and its potential relationship to the use of distal locking screw placement and whether there exists a relationship between the diameter of the CMN and the femoral canal.
(Left) Intra-operative fluoroscopy revealing proper proximal fixation during initial fixation. (Right) Three month post-operative film showing blade cut-out and catastrophic failure.
This study was approved by the Institutional Review Board (IRB). All patients initially treated with long cephalomedullary fixation for pertrochanteric hip fractures (OTA/AO 31A1, 31A2 or 31A3) between January 2003 and July 2014 at two level-1 trauma centers were identified by CPT codes 27245 (open treatment of IT, pertrochanteric or subtrochanteric femoral fracture with IM implant) or 27506 (open treatment of femoral shaft fracture). This cohort was further specified to patients who required one of the following additional procedure identified by the following CPT codes: 27245, 27506, 20680 (removal of hardware), 27132 (total hip arthroplasty), 27236 (hip hemiarthroplasty for fracture) or 27125 (elective hip hemiarthroplasty). These selection criteria yielded 46 patients.
Upon further review, fifteen patients were excluded for the following reasons: Nine patients had short cephalomedullary nails placed initially, three cases were coded incorrectly, one infection, one pathologic fracture, and one returned to the operating room for removal of a drain.
All operative notes were read by two residents to identify documentation of femoral canal reaming during the initial fracture fixation. Patient demographics abstracted from the medical record included age, gender, and laterality of the surgical site. BMI was separated into “overweight and obese” (BMI >25) and “normal” (BMI<25) based on World Health Organization guidelines.5
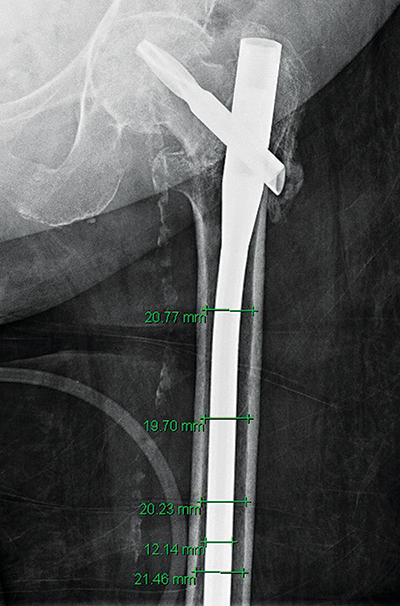
Surgical variables abstracted from the operative reports included number of distal locking screws, length of the implant and necessity of femoral canal reaming. Two residents performed radiographic evaluation of films pre- and post-operative to the initial procedure and all subsequent procedures. The films were examined for confirmation of the use of a long CMN initially, the number of distal locking screws and the ratio of femoral isthmus diameter to intramedullary implant diameter (Table 1). The femoral isthmus was defined as the narrowest portion of the femoral shaft as determined on postoperative AP plain radiographs. Measurement of the femoral isthmus was done using the measurement tool of radiographic viewing software (Centricity, GE Healthcare, Boston, MA). A minimum of four different measurements were taken on each radiograph to determine the narrowest inner cortical diameter. The diameter of the CMN was also measured and a ratio of the smallest endosteal (inner) cortical diameter measurement to the nail diameter was subsequently derived for each patient (Figure 2).
The primary outcome of interest was implant failure from migration of the proximal fixation device through the femoral head (blade cut-out). Secondary outcomes included implant failure that necessitated surgical revision/conversion for all other indications, including lateral thigh pain, distal femur pain and avascular necrosis of the femoral head. Continuous variable data were binned and all intergroup comparisons were performed using Fisher’s Exact Test. The isthmus/nail ratio distinction was set at 1.1 based on the common technique of over-reaming the femoral canal by 1mm greater than the size of the nail and was subsequently used for statistical analysis binning. A logistic regression model was used to calculate the odds ratio for intergroup comparisons of the number of distal screws placed. All data were analyzed using STATA software (Statacorp, LP. College Station, TX). Statistical significance was set at α < 0.05.
All CMNs utilized in this retrospective study were long and 11mm in diameter. Thirty-one (31) patients met the inclusion criteria for this study and the demographic data is summarized in Table 1. There were 10 (32%) male patients and 21 (68%) female patients. The mean BMI was 25.8 ± 1.2 kg/m2 with 5 (16%) overweight (BMI>30). Blade cut-out was the cause for revision/conversion in 18 (58%) patients. Removal of hardware for lateral thigh pain was the cause for revision/conversion in 8 (26%) patients. Removal of the distal locking screws for distal femur pain or loose screws was the cause of revision in 3 (10%) patients. Avascular necrosis and subsequent conversion to arthroplasty was the cause for revision in 2 (6%) patients.
The mean age of patients at the time of cephalomedullary nail fixation was 67.5 ± 4.0 years. There were 18 (58.1%) patients over the age of 65 in the study cohort. Age was found to have a significant association with revision for blade cut-out (p = 0.001).
The mean time to revision/conversion surgery was 10.1 ± 1.7 months and 21 (67.7%) patients required revision/conversion surgery within 12 months of initial CMN placement. Revision/conversion of the CMN for blade cut-out was more likely to occur within the first 12 months, which was a statistically significant association (p = 0.006).
Distal fixation varied within the cohort with 7 (22.5%) patients having no distal locking screws, 10 (32.3%) patients having one distal locking screw and 14 (45.2%) patients having 2 distal locking screws placed. The number of distal locking screws did not have a significant association with blade cut-out (p = 0.59). There was not a significant association when comparing zero distal locking screws and any distal locking screws with blade cut-out (p = 0.96).
There were 15 (48.4%) patients who did not have femoral canal reaming in preparation for nail insertion and there was a significant association with those who did not have canal reaming and failure due to blade cut-out (p = 0.03). A Fisher’s Exact Test was performed to determine if unreamed canals were associated with an isthmus/nail ratio >1.1. However, it did not demonstrate a significant association (p = 0.24).
The mean femoral isthmus/nail ratio was 1.24 ± 0.03 with one patient’s ratio absent as postoperative radiographs were unable to be obtained prior to revision from the medical record. The isthmus/nail ratio demonstrated a significant association with blade cut-out (p = 0.04) with an odds ratio of 6.48. (Table 2) summarizes the variables examined in this study and the statistical association with blade cut-out.
Patient demographic and technical factors affecting fixation failure rates of pertrochanteric hip fractures with intramedullary devices has been previously studied.3,4 Kashigar et al.3 and more recently Liu et al.6 demonstrated that the calcar tip-apex distance (CalTAD) is a predictor of proximal fixation cut-out when using CMN for PT fractures. However, the clinical significance of distal fixation in intramedullary constructs has not been previously examined. Biomechanically, one would expect changes to occur in the construct’s load sharing properties and rotational stability when distal locking screws are added. However, the published biomechanical studies are conflicting. Gallagher et al.7 concluded that locked CMNs have increased rotational load capacity with the suggestion that these constructs are more stable than their unlocked counterparts. Kane et al.8 showed similar peak torque strength of locked and unlocked CMN, suggesting either can be used without significantly changing the biomechanical properties of the construct. We initially hypothesized that a lack of distal fixation in a long CMN would allow a longer working length and therefore more stress on the proximal fixation leading to a propensity for cut-out. We did not, however, find an association with the presence of distal locking and blade cut-out in our data.
Perhaps the most striking observation in this data is that patients undergoing revision for blade cut-out were significantly more likely to have initially undergone CMN placement without sequential reaming of the medullary canal in preparation for nail insertion. The treatment of femoral shaft fractures with reamed nailing and larger diameter nails has been shown to decrease the rate of nonunion because of improved mechanical purchase and greater stability.9 In proximal femur fractures the femoral shaft/isthmus represents a potential point of distal fixation for intramedullary nails. As such, patients who underwent reaming of the canal may effectively have better qualitative bone density or smaller isthmic diameters and therefore require sequential reaming to insert the CMN device without excessive force. In such situations, reamed nails would result in the femoral shaft/isthmus acting as a point of distal fixation and thereby shortening the working area of the construct. Similarly, nail placement without canal reaming may occur in patients with more advanced osteoporosis, poorer bone quality, and more capacious canals, all factors potentially leading to an increased propensity for blade cut-out. This phenomenon was quantified by the observation that patients undergoing revision for blade cut-out were significantly more likely to have a isthmus/nail ratio of >1.1. This ratio serves as a way of assessing the degree to which the isthmus is acting as a distal point of construction fixation.
Age greater than 65 years was also noted to have a significant association with blade cut out (p = 0.001). This may relate to decreased bone mineral density with increasing age.10-12 This is supported by the significant association we found between age > 65 years and isthmus/nail ratio >1.1 (p = 0.045). Additionally, blade cut-out requiring revision or conversion of the implant was significantly more likely to occur within the first postoperative year (p=0.006). There are a number of factors that affect this finding from technical aspects of the surgical fixation (quality of reduction, CalTAD, etc.) to patient-related factors such as development of AVN and poor bone quality.11,13,14 This association underscores the necessity to optimize surgeon controlled variables, such as fracture reduction and location of the proximal fixation device.
There are several limitations to this study, the most significant of which is the overall small size of the cohort, which potentially creates type 2 error. Additionally, the low incidence of blade cut-out or fixation failure of CMN for PT fractures reported between 1.9% and 2.9% makes this a challenging area to investigate.14,15 Moreover, the practice of placing distal locking screws is largely dependent on surgeon preference irrespective of patient factors. Consequently, a randomized prospective model may be the only truly effective way of evaluating the utility of distal locking screw constructs.
Failure of cephalomedullary nail fixation for pertrochanteric femur fractures is a distressing complication. Blade cut-out is a common form of failure with other studies identifying technical factors leading to increased risk of failure. We have introduced, from a small sample set, that the effective working length of the CMN, namely whether isthmic purchase is present, may be an important consideration during the treatment of these fractures. This is particularly important given that many surgeons do not frequently ream and typically utilize only a single size CMN implant for all femoral canal sizes. Thus, this preliminary study begins to explore whether older, osteoporotic patients with larger femoral canals would benefit from the use of CMNs whose diameter is determined at the time of surgery based on the nascent canal size. By sizing the implant to the isthmus, a shorter working area would be created and might reduce the failure rate from blade cut-out.