Failure of Consolidation of a Peri-Articular Distal Tibial Bone Cyst Post Curettage due to Communication with the Ankle Joint
Eric C. Loesch, BS, Ankur B. Bamne, MBBS, MS, John Y. Kwon, MD
Disclosure Information©2015 by The Orthopaedic Journal at Harvard Medical School
Curettage and bone grafting is the standard of care for benign cystic bony lesions. We report a case in which bony consolidation of a peri-articular bony cyst failed to occur because of a communication with the ankle joint and seepage of synovial fluid into the cyst. We also describe a method to manage such a case. Peri-articular benign bone cysts may fail to consolidate following curettage and bone grafting due to communication with a joint. It is important to remove this communication with the joint to ensure adequate healing of the cyst.
Tumors of the foot and ankle region are rare and constitute 1-2% of all bone tumors.1 Benign bone tumors are more common than malignant tumors with a ratio of 4:1.2 Benign lesions are slow growing and often present as an incidental finding. Curettage and bone grafting has been the standard of care for benign lesions if operative treatment is required. In some instances, peri-articular lesions may communicate with the joint making treatment much more difficult. Non-invasive modalities like CT and MRI are often used to assess such a possibility.3
We present the case of failed consolidation of a peri-articular benign cystic lesion due to communication with the ankle joint. The cyst was subsequently managed by osteotomy, excision of the communicating tract, bone grafting and fixation.
A 25 year old female who initially sought consultation for an ankle sprain was diagnosed with a benign bony lesion in the right medial malleolus. She was treated with curettage and bone grafting at an outside institution, along with bracing and non-steroidal anti-inflammatory drugs (NSAIDs) post-operatively. Biopsy revealed a benign lesion. Several months after her surgery, the patient’s pain persisted. Her symptoms were aggravated by standing and walking, with partial relief during rest. She subsequently underwent a second similar procedure but reported continued pain. She was referred to our institution due to persistent daily pain, disability, and difficulties with activities of daily living. On physical examination, she had a well-healed scar over the postero-medial aspect of her right ankle and tenderness over the antero-medial joint line of the same ankle. Both sensation and perfusion to the extremity were intact.
Plain radiographs revealed a radiolucent lesion in the medial malleolus (Figure 1). Advanced imaging demonstrated a communication with the ankle joint through a bony defect in the subchondral bone of the distal tibia (Figure 2). The cyst cavity was incompletely consolidated.


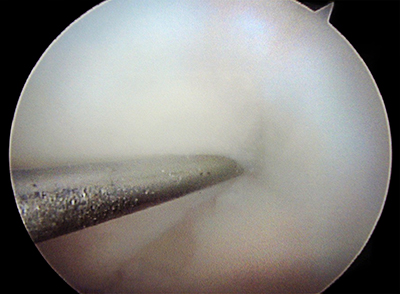
A routine ankle arthroscopy was performed first using standard antero-medial and antero-lateral portals. Mild synovitis was present. Over the medial aspect of the tibial plafond, there was fissuring noted of the cartilage. A defect was confirmed with a probe, which was consistent with findings on multiple imaging studies. It was determined that the cyst cavity was communicating with the joint through this defect in the articular cartilage and subchondral bone (Figure 3).
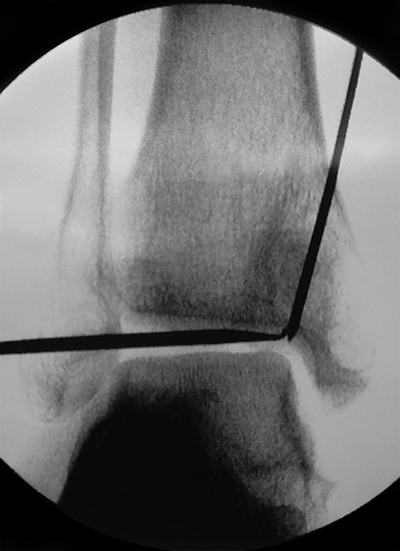
Before the medial malleolar osteotomy, a K-wire was drilled under fluoroscopic guidance from the proximal aspect of the medial malleolus into the joint to meet the probe at the level of the joint. This was the site of the osteotomy, which was planned in order to remove the communication between the cyst and the joint (Figure 4). Next, the osteotomy was hinged open, taking care to maintain the continuity of the deltoid ligament. The cyst cavity was curetted out with incomplete consolidation of previous bone graft material noted. Infection was ruled out via intra-operative frozen section. Autologous cancellous bone graft was then harvested from the proximal tibia, mixed with demineralised bone matrix and packed into the cyst cavity. The osteotomy was reduced and provisionally fixed with K-wires. Intra-articular reduction and articular congruity was confirmed by arthroscopy. Final fixation was done using a contoured one-third tubular plate and two 3.5mm cortical screws inserted across each fragment. Although the distal most screw appeared close to the ankle joint on intraoperative fluoroscopy, direct arthroscopic examination of the plafond revealed the screw to be extra-articular. Closure was performed in layers and a splint was applied. The patient remained non weight-bearing for 3 months following the procedure.
At her 6-month follow-up visit the patient was bearing full weight on the affected extremity and did not complain of any pain. She was able to resume her daily activities without any restrictions. On examination, there was no tenderness around the ankle and her range of motion was noted to be from 10 degrees dorsiflexion to 40 degrees plantarflexion. Radiographs revealed that the cyst was well-consolidated (Figure 5).

Curettage and bone grafting is the standard of care for benign bony lesions. In such cases, the cyst is packed with bone graft in an attempt to consolidate the bony cavity. Less clear, however, is the management of a bone cyst communicating with the adjacent joint. In our case, perforation of the subchondral bone led to seepage of synovial fluid into the cavity. Synovial fluid is known to contain anti-angiogenic factors which inhibit bony healing.4 Whether the defect was a result of surgical trauma or secondary to the cyst perforating the joint is not known. Buchler et al. reported five cases of intra-osseous ganglion cysts communicating with the ankle joint via a chondral flap.5 In their series, they probed all of the lesions and each of the five cysts healed without complication. In our case, it was critical to obliterate the communication between the cyst and the joint in order to ensure adequate healing of the cyst. This was accomplished by executing the osteotomy in a way that removed this defect. Arthroscopic guidance of our k-wire allowed for a precise cutting guide for our planned osteotomy directly towards the lesion. Knowing that the defect was approximately 2 mm in diameter based on preoperative imaging and arthroscopic conformation, a saw blade with a 2 mm width was selected. When directed at the lesion, the removal of bone by the saw blade removed the defect and resulted in two congruent edges upon closure of the osteotomy. The articular congruity was ensured by arthroscopy and stable fixation of the osteotomy was achieved with internal fixation.
In summary, the key to managing a peri-articular bone cyst is to identify the subchondral defect and communication with the joint, plan the osteotomy in such a way so as to remove the defect, check the articular congruity using arthroscopy, and ensure stable internal fixation. Advanced imaging such as CT or MRI (+/- arthrogram) is recommended and thin-cuts or 3-Tesla imaging may be required to identify suspected lesions. If lesions without known intra-articular communication fail to heal but no communication is visualized on advanced imaging, arthroscopy should be strongly considered to allow for direct visualization of the articular surface.