Rehabilitation Variability After Biceps Tenodesis
Michael D. Galetta, BS, Timothy T.W. Cheng, MD, Rachel E. Keller, BS, Elan Harris, BS, Luke S. Oh, MD
The authors report no conflict of interest related to this work.
©2021 by The Orthopaedic Journal at Harvard Medical School
BACKGROUND There is limited data to guide postoperative rehabilitation protocols after biceps tenodesis (BT). The lack of concensus is concerning, especially since publicly available BT rehabilitation protocols are becoming more accessible to patients online. In an effort to understand current practice, an analysis of publicly available BT rehabilitation protocols is warranted. The objective of this study is to evaluate the variability among publicly available BT postoperative rehabilitation protocols.
METHODS An internet search was conducted for publicly available BT rehabilitation protocols from websites of all Accreditation Council for Graduate Medical Education (ACGME) academic orthopaedic institutions. A supplemental ten-page Google search was also performed with the search terms “biceps tenodesis rehabilitation protocol”. Collected protocols were examined for information relating to the following rehabilitation guidelines: acute postoperative management, range of motion, strengthening, and return to sport/unrestricted activity. Main outcome measures were descriptive statistics.
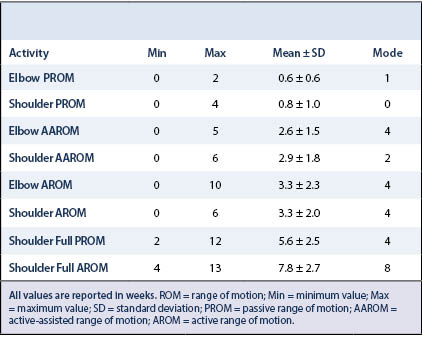
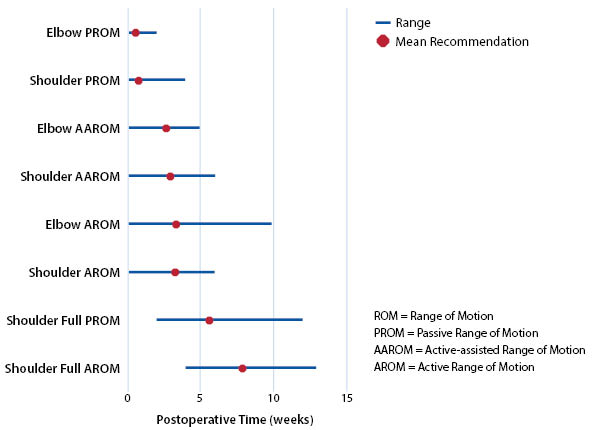
RESULTS Thirty-three rehabilitation protocols were inluded for analysis. Shoulder active range of motion (AROM) initiation ranged from 0-6 weeks ([mean] 3.3 weeks). Elbow AROM initiation ranged from 0-10 weeks (3.3 weeks). Achievement of full shoulder passive range of motion (PROM) and AROM varied between 2-12 weeks (5.6 weeks) and 4-13 weeks (7.8 weeks), respectively. Initiation of shoulder strengthening ranged anywhere from 0-12 weeks. Initiation of elbow strengthening varied between 4-12 weeks.
CONCLUSION Postoperative rehabilitation protocols for BT are lacking consensus. This study highlights the variability of clinical recommendations among online available BT rehabilitation protocols. Additional research is needed to develop evidence-based guidelines for BT rehabilitation.
LEVEL OF EVIDENCE Level IV
KEYWORDSBiceps tenodesis; shoulder; elbow; rehabilitation; range of motion; strengthening; return to sport
The long head of the biceps (LHB) tendon is a common source of anterior shoulder pain for many patients.1-4 There is a variety of LHB tendon pathology that can lead to pain including inflammation, degenerative tears, tears at the superior labral origin, and LHB tendon instability.1,3,5 Additionally, patients with LHB pain often have concomitant pathology such as rotator cuff tears, subacromial bursitis and impingement, labral tears, and glenohumeral arthritis.2-7 Initial treatment for LHB pathology is usually nonoperative in nature including rest, activity modification, physical therapy, nonsteroidal anti-inflammatory drugs, and corticosteroid injections.5-7 For patients who do not respond to conservative care, operative management can be considered and includes tendon debridement, biceps tenotomy, and biceps tenodesis (BT).5,7,8
Biceps tenodesis is a common surgical procedure that has grown in popularity after its indications expanded to include SLAP tears.9-11 Werner et al. described an increase in BT frequency from 2008 (8,178 procedures) to 2011 (14,014 procedures).6 High case volumes for BT may be related to its association with rotator cuff tears4,6 – a condition that is estimated to affect 20.7% of the general population12 and concomitantly treated in 82.1-93.3% of BT cases.6
Increasing prevalence of BT has led to adoption of different surgical techniques, approaches, and fixation methods.5,7,13,15 Many cadaveric biomechanical studies have been conducted to evaluate the strength of various fixation methods;13,16 however, the application of these data are limited since the fixation strengths required for various activities are not explicitly known.
With little to no evidence to base BT rehabilitation guidelines, we question the state of BT rehabilitation in our collective practices. To our knowledge, only one study has specifically compared postoperative rehabilitation guidelines to outcomes after BT.17 This dearth of information is problematic considering the clear benefits to the standardization of medical care.18-23 For a procedure that affects so many people, it is critical for us to identify the extent of our variation regarding BT rehabilitation.
Given the limited evidence available to guide BT rehabilitation, the purpose of this study was to review publicly available BT rehabilitation protocols and evaluate the variability in their guidelines. By understanding the variation amongst these protocols, we hope to identify the recommendations which need more supporting evidence.
The Electronic Residency Application Service (ERAS) was used to identify ACGME-accredited academic orthopaedic institutions. Additionally, the San Francisco Match (SF Match) was used to identify ACGME-accredited sports medicine fellowships without an associated residency. From these methods, we created a list of every ACGME-accredited academic orthopaedic/sports medicine program.
In January of 2020, the authors searched each program’s website for the presence of publicly available BT rehabilitation protocols. Any BT rehabilitation protocols that were found were collected for screening. If no protocols could be found, the authors performed a Google search of the institution’s name followed by “biceps tenodesis rehabilitation protocol”. Protocols resulting from this search were included only if they were affiliated with the institution specified in the Google search.
After all institutional protocols were collected, the authors conducted a supplemental Google search with the terms “biceps tenodesis rehabilitation protocol”. All BT rehabilitation protocols resulting from the first ten pages of this search were collected
The collected protocols were then screened to exclude duplicate protocols, protocols published outside of the United States, and/or protocols describing concomitant procedures (e.g. rotator cuff tear). Of the remaining included protocols, data were extracted for the following categories: protocol demographics, acute postoperative management, range of motion (ROM), strengthening, and return to sport (RTS)/unrestricted activity.For protocol demographics, the authors collected each protocol’s institution and year of protocol publication. Regarding acute postoperative management, initiation of formal physical therapy and time to sling discontinuation were extracted. For ROM, initiations of passive range of motion (PROM), active-assisted range of motion (AAROM), and active range of motion (AROM) for both the shoulder and elbow were collected. Additionally, time to full shoulder PROM and AROM were noted. Next, strengthening was measured by initiations of shoulder isometric strengthening, scapular stabilizer strengthening, shoulder resistance training, elbow flexion strengthening, and elbow pronation/supination strengthening. Lastly, RTS/unrestricted activity was analyzed by extracting the initiations of plyometrics, throwing, sports-specific drills, and time to physician clearance for full activity. If time points for rehabilitation guidelines were provided as ranges (i.e. 6-12 weeks), the earliest time point was used for guidelines of initiation (i.e. PROM initiation, strengthening, plyometrics, etc.) and the latest time point was used for guidelines on full ROM achievement.
Descriptive statistics such as the mean, standard deviation, range (minimum and maximum time points), and mode were used to describe the collective recommendations made by the included protocols.
Protocol Demographics
Thirty-three rehabilitation protocols were included for analysis. Of the 187 ACGME accredited orthopaedic residency programs, only 28 (15.0%) of them had protocols publicly available online. An additional five protocols (20.8%) were found from ACGME accredited sports fellowship programs. Protocols were published between 2003 and 2019.
Acute Postoperative Management
Thirty-two (97.0%) rehabilitation protocols started formal physical therapy within the first 2 weeks (mean: 1.0±1.2 weeks; range: 0-6 weeks). One program did not start formal physical therapy until six weeks postoperatively. Thirty-two (97.0%) rehabilitation protocols recommended the use of slings, recommending discontinuation at an average of 3.7±1.5 weeks (range 1-6 weeks).
Range of Motion
Detailed results for range of motion guidelines are reported in Table 1 and represented in Figure 1. Twenty-nine (87.9%) protocols initiated shoulder PROM within the first week, and all (100%) protocols initiated elbow PROM within 2 weeks. For shoulder AROM, nine (27.3%) protocols recommend initiation within the first week, but an additional nine (27.3%) protocols recommended initiation after 5 weeks. Eighteen (54.5%) of the collected protocols endorsed elbow AROM after 4 weeks, yet eight (24.2%) protocols endorsed elbow AROM within 1 week. The ROM guidelines with the largest reported ranges were elbow AROM initiation (0-10 weeks), time to full shoulder PROM (2-12 weeks) and time to full shoulder AROM (4-13 weeks).
Strengthening
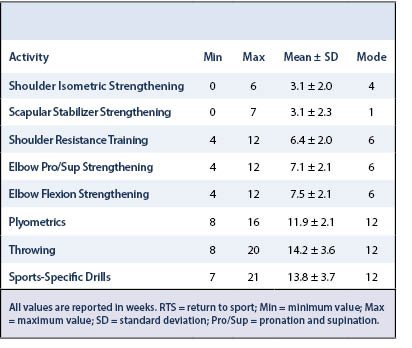
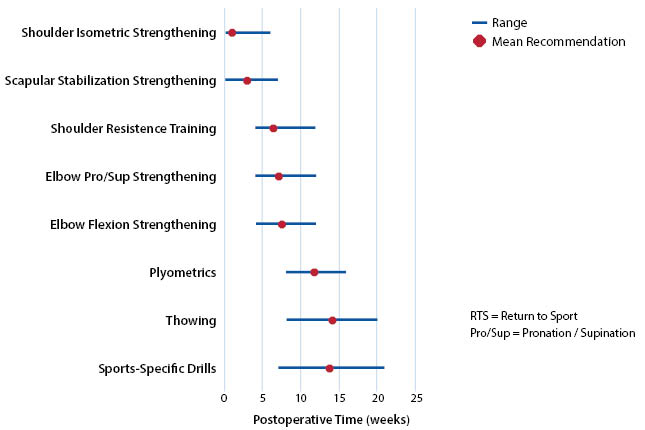
Detailed results for strengthening guidelines are reported in Table 2 and represented in Figure 2. All strengthening modalities started at 6 weeks or later. Interestingly, scapular stabilizer strengthening was found to have a two-week discrepancy between its mean (3.1 ± 2.3 weeks) and its mode (1 weeks). The only other rehabilitation guideline to exhibit this discrepancy was throwing (mean: 14.2 ± 3.6 weeks; mode: 12 weeks).
Return to Sport/Unrestricted Activity
Twenty-eight (84.8%) protocols included information pertaining to RTS/unrestricted activity, either in the form of timing of sports-specific drills, initiation of a throwing program, plyometric drills, or recommendations for return to full activity. Detailed results for RTS are reported at the bottom of Table 2 and represented at the bottom of Figure 2. Time of expected physician clearance for full activity was provided in twelve of the protocols at an average of 20.4 ± 7.7 weeks (range: 12-36 weeks). Twelve protocols mentioned physician clearance as a requirement for full activity clearance. Seven of these twelve protocols also provided an expected time point for RTS. The remaining five protocols solely relied on physician clearance and gave no timeline for RTS.
Rehabilitation after BT surgery plays a crucial role in restoring pain-free function and returning patients to their desired level of activity. Despite the increasing popularity of this procedure,6,9–11 there is a lack of biomechanical and outcome data available to support clear ROM, strengthening, and RTS/unrestricted activity guidelines. Further, postoperative rehabilitation is an important factor when patients consider undergoing surgical treatment. Galdi et al. showed that longer recovery times are a significant factor for patients choosing to forego a BT in favor of a biceps tenotomy (Odds Ratio 1.69, p = 0.001).8 Given this information, it is imperative to analyze:
- What we are asking patients to do during rehabilitation
- Why we are asking them to do it
In an age without standardization of BT rehabilitation, it is critically important to evaluate the variability among BT rehabilitation protocols. By understanding the variation amongst these protocols, we can identify the rehabilitation guidelines that require evidence-based answers.
Clinical Consensus
Clinically, there does appear to be some consensus amongst the protocols. The main consensus was observed in initiation of formalized physical therapy and PROM for both joints. All protocols (except one) recommended early physical therapy starting within the first 2 weeks. Twenty-nine protocols endorsed starting shoulder PROM within the first week of rehabilitation and all thirty-three protocols recommended elbow PROM within the first two weeks. Although recommendations could always be more standardized, these recommendations seem to be, more or less, agreed-upon clinically.
Clinical Variability – Acute Postoperative Management
Variability in the rehabilitation protocols was observed in all other parameters. Regarding acute postoperative management, there was a 5-week range (1-6 weeks) for discontinuing sling use. It is unclear, however, what effect length of sling wear has on long-term patient outcomes given the lack of literature in this area.
Clinical Variability – Range of Motion
While PROM initiations exhibited some clinical consensus, agreement fades as rehabilitation progresses to other ROM guidelines. AROM guidelines for the shoulder and elbow were markedly variable amongst protocols. Shoulder AROM ranged from 0-6 weeks, while elbow AROM ranged from 0-10 weeks. For shoulders, 27.3% of protocols recommend starting AROM within the first week and 27.3% recommended starting after 5 weeks. For elbows, initiation of AROM was even more variable. While 54.5% of the collected protocols endorsed elbow AROM after 4 weeks, almost a quarter (24.2%) of them endorsed elbow AROM within 1 week postoperatively.
There was also clinically relevant variation regarding achievement of full shoulder ROM (in all planes of motion). Full shoulder PROM is prescribed within a range of 2-12 weeks, while full shoulder AROM is prescribed within a range of 4-13 weeks. The clinical significance of 9+ weeks in an acute postoperative rehabilitation setting is quite substantial, and these findings warrant concern.
Clinical Variability – Strengthening
Similarly, there was variability in initiation of all strengthening exercises. No strengthening modality started earlier than 6 weeks. Again, these discrepancies are clinically concerning in the acute rehabilitation setting considering the differences in healing progression between these time points; yet, it remains unclear what effect the variation in strengthening initiations has on patient function and outcomes.
Clinical Variability – Return to Sport/Unrestricted Activity
Clinical variability was also seen in rehabilitation guidelines for sports-specific activity and full RTS. The largest range was observed for clearance for full activity, which ranged from 12-36 weeks. Moreover, initiations for plyometrics, throwing, and sports-specific drills also had large ranges of 8, 12, and 14 weeks, respectively. While it may be reassuring to counsel patients with specific timelines for their RTS, there are no evidence-based guidelines to support accurate, yet generalized, estimations for RTS at this time. Lastly, over a third of protocols reviewed (36.3%) required physician clearance for full activity, s that some aspect of the protocol likely needs to be individualized to the patient. This observation also alludes to a potential tendency of providers to rely heavily clinical judgement rather than evidence-based rehabilitation guidelines for BT.
Biceps Tenodesis Rehabilitation Protocol Considerations
There are many factors to consider when designing a BT rehabilitation protocol. Many of the rehabilitation protocols reviewed for this study explain that the reasoning behind their regimen was to balance protection the surgical repair and restoration of physical function, as is common in rotator cuff repair literature.24-27 As such, the timing of the rehabilitation guidelines is set to allow for progression of activities as biological healing occurs. Preferences of some surgeons/institutions to favor protection over function (or vice-versa) may lead to conflicting recommendations between two protocols for the same condition.
Another important factor to discuss when considering postoperative rehabilitation protocols is symptomatic progression of the patient. While structural integrity of a repair is important to consider, restricting certain activities at various time points may also affect postoperative pain and subsequently their functional recovery/outcomes. Therefore, it is important to adequately balance the needs of the patient with the needs of the repair. How to do so effectively will hopefully become the subject of future studies – ones that compare BT rehabilitation guidelines with outcomes.
To our knowledge, one singular study addresses BT outcomes as it relates to postoperative BT rehabilitation protocols. Liechti et al. (2018) investigated objective clinical outcomes of patients who had no postoperative restrictions after BT.17 In this study, 105 patients (109 shoulders: 72 male, 37 female) underwent primary open BT with a bicortical suture button and interference screw construct. They initiated physical therapy immediately and were able to perform ROM and strengthening exercises as tolerated. Patients were allowed to return to athletic activities once pain free. After an average of 3.5 year follow-up (minimum 2 years), Liechti et al. found a failure rate of 2.2% and overall high levels of function on patient reported outcome measures.17 Interestingly, their failure rate seems to be consistent rates described in the literature6,7,28 despite having no postoperative restrictions. While this study does provide some evidence that good outcomes after BT can be obtained without postoperative restrictions, there was no control group in this study to allow us to determine if this is the optimal strategy. Ultimately, more research is needed to help build evidence-based recommendations that either support or reject these types of recommendations.
Overall, the differences in rehabilitation guidelines for BT are quite concerning. Variations in recommendations by multiple weeks is clinically significant for BT healing and proper restoration of function. Further, the state of the supportive literature is also bleak. Contrary to the popularity of this procedure, evidence-based rehabilitation guidelines for BT rehabilitation are lacking and require further research. Doing so would move us on a path to standardization, resulting in better outcomes for the patient, increased efficiency for surgeons, and decreased burden on the healthcare system as a whole.18-23
Limitations
This study is the first to evaluate the variability of published rehabilitation protocols for BT. This study needs to be assessed in light of its limitations. One limitation of the study is that we only evaluated publicly available BT protocols so any protocols that were individually distributed to patients or physical therapists were not included. Additionally, while we did try to create a systematic method to search for rehabilitation protocols, it is possible that a publicly available protocol was available but not found in our search. While this may have potentially decreased the number or protocols reviewed, it does represent what a patient or physical therapist may experience when performing their own internet search for an online BT rehabilitation protocol after surgery. Additionally, many surgeons may have their own private/dictated protocols which are not published publicly online. These protocols may hold different recommendations than those reported in our study’s cohort; however, our study was designed to simulate what can be easily found and referenced online.
Another limitation of our study is that we did not separate protocols based on surgical technique. While this may make a difference, there are no data in the literature supporting that outcomes are different based on rehabilitation protocol and surgical technique. Lastly, there was no consensus statement or gold standard BT rehabilitation protocol for us to statistically compare our results to; however, this is a limitation that was, ironically, a motivation for this study. Due to the lack of consensus surrounding BT rehabilitation, we believed it was critical to:
- Evaluate the current state of BT rehabilitation
- Identify research gaps for development of future evidence-based rehabilitation guidelines
From this study, we hope more surgeons will note the various areas of need and fill them accordingly with future research.
The majority of postoperative rehabilitation for BT is lacking consensus. This study highlights the variability of clinical recommendations among online available BT rehabilitation protocols. Gaps in the literature have been presented, allowing for future impactful research studies and the development of evidence-based guidelines for BT rehabilitation.