Quantifying Rotational Instability in Ulnar Collateral Ligament Injuries of the Thumb: A Cadaveric Study
Farhan Ahmad, BS, Patrick G. Marinello, MD, Jennifer Peterson, MD, Steven Maschke, MD, Xavier Simcock, MD
©2021 by The Orthopaedic Journal at Harvard Medical School
BACKGROUND Injuries to the ulnar collateral ligament alter thumb metacarpal phalangeal (MCP) joint biomechanics. We hypothesized that sequential disruption of the dorsal capsule and proper ulnar collateral ligament (pUCL) followed by the accessory ulnar collateral ligament (aUCL) of the thumb MCP would lead to progressive rotational instability.
METHODS Twelve fresh-frozen adult cadaveric upper extremities with intact thumbs were used for this study. Under fluoroscopy, two 0.45 Kirshner wires were placed parallel to the MCP joint through the distal metacarpal and proximal phalanx, approximately 2 cm from the joint. The dorsal capsule and pUCL followed by the aUCL were sequentially sectioned. The MCP joint range of motion was measured in pronation and supination with the hand in natural resting position using a digital goniometer.
RESULTS After sectioning the dorsal capsule and pUCL, the mean pronation and supination were 23.4°±8.8° and 21.6°±3.4° respectively, which increased to 28.2°±9.2° and 29.7°±2.6° respectively after additionally sectioning the aUCL (P<0.05). With the pUCL sectioned, the mean percentage increase in pronation and supination was 29.2%±14.8% and 39.2±22.4%, respectively, compared to baseline. With the aUCL also sectioned, the increase in percentage pronation and supination from baseline was 41.6%±12.8% and 57%±12.9%, respectively.
CONCLUSION This biomechanical study demonstrates a significant increase in the rotational instability (pronation and supination) of the metacarpal phalangeal joint after UCL injury. Clinically, this increase in rotational instability may help diagnose UCL injuries of the thumb more accurately and supplement traditional valgus stress testing of this injury.
LEVEL OF EVIDENCE Level V Cadaveric Study
KEYWORDS UCL Injury; rotational instability; cadaveric study; skier’s thumb; gamekeeper’s thumb
Injuries to the ulnar collateral ligament (UCL) can result in altered biomechanics of the thumb metacarpal phalangeal (MCP) joint.1 The metacarpal phalangeal joint of the thumb is a diarthrodial joint that allows for six degrees of motion: flexion, extension, abduction, adduction, pronation, and supination.1,2 Classically, UCL injuries are thought to result in mainly valgus instability of the MCP joint after a valgus stress injury. However, it is essential to note that rotational forces also play a role in the mechanism of injury. During an injury, a spectrum of disruption can occur—first disrupting the dorsal capsule and proper ulnar collateral ligament (pUCL) and then disrupting the accessory ulnar collateral ligament (aUCL).3
During clinical evaluation, valgus instability is a pathognomonic diagnostic finding consistent with UCL injury.4 In an uninjured thumb, there is minimal rotation about the MCP joint, but injury of the medial ligamentous structures leads to increased rotation about the MCP joint. Several studies have highlighted that the UCL is a rotational stabilizer in MCP joint disarticulation models.5,6 It has been our clinical experience that general rotational instability of the injured MCP thumb joint is equally as helpful as valgus instability in making the diagnosis. Testing for increased pronation and supination with the thumb and hand in a resting position has been a consistent finding with UCL injury in our clinical practice. Furthermore, it has been our experience that rotational instability testing is also valuable for gauging recovery and return to work or sports after operative treatment.
The purpose of our study was to substantiate our clinical findings with a cadaveric model that would simulate clinical examination of an injured thumb. Our hypothesis was that sequentially disrupting the proper ulnar collateral ligament (pUCL) and the accessory ulnar collateral ligament (aUCL) of a thumb will lead to significant progressive rotational instability.
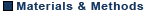
Twelve fresh-frozen adult cadaveric upper extremities with intact thumbs were used for this study. Thumbs were examined physically to ensure no sign of prior incision or surgery and clinically to ensure no laxity. The mean age was 65 years (range 49-76), with four female and eight male specimens. The specimens were thawed to room temperature prior to testing. The same single fellowship-trained orthopaedic surgeon conducted the study, including sectioning and measuring. All the specimens were placed in a vice grip in the same position on the table and then dissected to expose the dorsal capsule, the pUCL and the aUCL on the medial side of the thumb (Figure 1). Under fluoroscopy, two 0.45 Kirshner wires (K-wire) were placed through the distal metacarpal and proximal phalanx, approximately 2 cm from the MCP joint (Figure 2). These wires were placed parallel to the joint line and parallel to the horizon of the working table surface. A digital camera was mounted 48 cm behind the experiment set-up, perpendicular to the K-wires. Under standard testing conditions, the MCP joint was pronated and supinated using the K-wires as joysticks to maximal ROM. Each specimen was conditioned through 10 cycles of pronation and supination prior to testing in a manner similar to actual patients in the clinical environment.

The dorsal capsule and pUCL followed by the aUCL were sequentially sectioned, and the MCP joint was ranged manually in pronation and supination in the natural resting position of the hand. Maximal pronation and supination were determined by ensuring there was no deformation of the K-wires. The relative pronation and supination between the proximal phalanx and the metacarpal were measured by three independent examiners using a digital goniometer. The axis of the K-wire in both the proximal phalanx and the metacarpal were used to determine the angle to the nearest degree.
Statistical analysis
The mean values were used for data analysis. Each specimen served as a control for the experimental conditions since we obtained baseline testing prior to sectioning. A Student’s paired t-test was used for statistical analysis setting a P<0.05 as statistically significant.
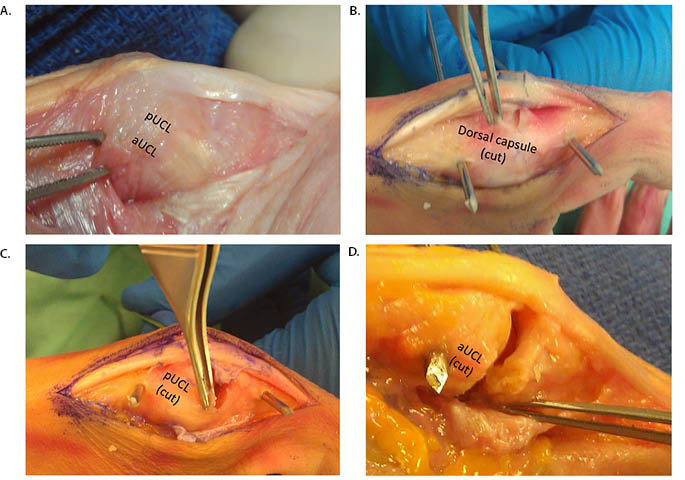
Mean baseline pronation and supination was 15.7°±4° and 12.6°±3.9°, respectively.
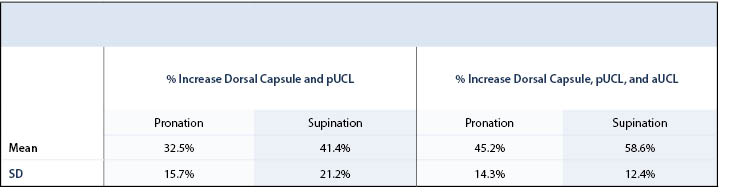
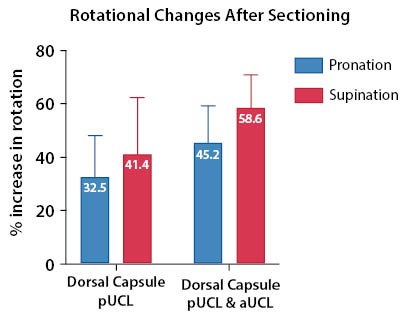
After sectioning the dorsal capsule and pUCL, the mean pronation and supination was 24.1°±8.1° and 22.1°±3.3°, a mean relative increase in pronation of 32.5%±15.7% and supination of 41.1%±21.2% compared to baseline (p<0.05). After sectioning the aUCL, mean pronation increased to 29.8°±9.1°, and supination increased to 30.5°±3° (Table 1). With the aUCL also sectioned, the increase in percent pronation and supination from baseline was 45.2% (SD 14.3%) and 58.6% (SD 12.4%), respectively, both of which were statistically significant (P<0.05) (Table 2 and Figure 3).
This biomechanical study assessed the rotational (pronation and supination) instability of the MCP joint after sequential UCL sectioning using 12 fresh-frozen cadavers. After sectioning the dorsal capsule and the pUCL, there was a statistically significant increase in pronation and supination, which further increased after sectioning of the aUCL. These findings suggest that the UCL is an important contributor to the rotational stability of the MCP joint.
There is a clinical utility for this observation. The acute diagnosis of a complete rupture of both the aUCL and pUCL is still the primary burden of the hand surgeon when a patient presents with an injury to the thumb MCP joint. The accuracy in making the diagnosis between complete and partial tears holds a significant impact for the patient. The treatment algorithm relies on the diagnosis of complete versus partial tears. Accurate and reliable physical diagnosis becomes even more critical in our cost-conscious medical system. With a proper clinical diagnosis, advanced imaging can be more judiciously used. Furthermore, rotational instability may be useful to gauge recovery and return to work or sports after operative treatment.
Partial tears have a much higher chance of successful treatment with immobilization alone than complete tears.4,7 The success of non-operative treatment quickly decreases if there is a complete tear, especially with interposition of tissue.7 Already the clinical and diagnostics tools to quantify the degree of tear have been broadly investigated.8-11 The general opinion is that greater than 30° of a valgus laxity without a clear endpoint, as well as an increase of 15° asymmetry to the contralateral uninjured side, indicate a complete tear of both the accessory and proper ligaments.4 The accuracy can be further increased with fluoroscopy.11 The flexion biomechanics of this injury has been thoroughly established in the resulting valgus instability.9,12 Furthermore, this has recently been quantified in regards to the rotational contribution to valgus instability.5
The utility of measuring valgus instability alone has been questioned, primarily because no clear consensus has emerged as to the cut-off angle for a complete tear clinically without fluoroscopy.4,10,11 Recently, the presumption that the contralateral thumb stability is symmetric in control patients has also been examined. A clinical study conducted at the University College of London established that there is little correlation between right and left thumbs in normal individuals.4 Surprisingly, 34% of individuals have a difference in abduction of 10° at least.
However, to our knowledge, no previous investigation has focused on rotational instability alone. Since a complete tear of both aUCL and pUCL results in instability in two planes (coronal and axial), we believe this could provide a clinical clue before undergoing additional radiographic tests. Furthermore, the difference in rotation for a complete tear in both supination and pronation of 45.2% and 58.6% leads to a significantly increased total arc of rotation, which we believe may be clinically detectable with a manual exam.
The weaknesses of this study are that it is a biomechanical cadaveric study, and it has not been validated clinically. Additionally, the study was not blinded, so it is possible that examiners applied variable forces depending on the testing conditions. Future studies should repeat this experiment with blinded examiners or a custom jig that can standardize applied forces to validate results. The design of our study was constructed to simulate clinical testing. Manual pressure was used to measure the rotational change with serial sectioning. Only a limited dissection of the thumb was completed, with previous studies that have investigated the role of rotational instability in UCL injury have used disarticulated thumb models. We chose to use complete upper extremities placed in the resting position on a table. Only a small number of specimens were assessed, and the effects of freezing on tissue compliance could not be determined, although this model has been described previously.
This biomechanical study demonstrates a significant increase in the rotational instability (pronation and supination) of the metacarpal phalangeal joint after UCL injury. The findings highlight the important contribution of rotational instability alone in this injury. Clinically, this increase in rotational instability may help more accurately diagnose a gamekeeper’s thumb and supplement traditional valgus stress testing of this injury.