History of HCORP: The Harvard Combined Orthopaedic Residency Program
James H. Herndon, MD, MBA
The authors report no conflict of interest related to this work.
©2018 by The Orthopaedic Journal at Harvard Medical School
The Harvard Combined Orthopaedic Residency Program (HCORP)–founded in 1921–has had a long and rich history. In its 97 years, the program has been overseen by eight successive program directors, each of whom has had a strong commitment to education. More recently, the Harvard Orthopaedic Executive Committee has also provided input.
Faculty, residents, fellows, medical students and program graduates have made significant contributions in orthopaedic surgery and have been leaders in orthopaedics locally, regionally, nationally and internationally.
This paper briefly summarizes the complex history of the residency program and some of the milestones and significant changes that were influenced by each of the program directors.
LEVEL OF EVIDENCE N/A
KEYWORDSHarvard Orthopaedic Residency, history, residency program directors
On November 22, 1782 the Harvard Corporation voted to “form…[a] Medical Institution on the subject of conferring medical degrees.” Dr. John Warren was asked to develop a course of studies. His first course (six weeks in length) included lectures and demonstrations on each of the following topics:
- OSTEOLOGY, or a definition of the Bones
- MYOLOGY, of the muscles
- SPLANCHNOLOGY, of the Viscera contained in the large Cavities
- ANGEIOLOGY, of the Blood Vessels and Lymphatics
- NEUROLOGY, of the Nerves
- ADENOLOGY, of the Glands
After Dr. John Warren’s death in 1815, lectures on bones, joints and muscles were delivered by his son, John Collins Warren-cofounder of MGH and its first chief of surgery-who had a fascination with skeletons.
Harvard’s medical school was the third medical school in the United States. The first was founded in Philadelphia in 1765 at the College of Philadelphia (now the University of Pennsylvania) and the second was started in 1767 at King’s College in New York (now Columbia University College of Physicians and Surgeons). The majority of physicians practicing in the United States before the opening of these medical schools served apprenticeships with practicing physicians in the United States or studied in Europe. Graduates of the newly opened medical schools in Philadelphia, New York and Boston entered private practice or served an apprenticeship (six months – two years) with a practicing physician before starting their own practice. Some also studied further in Europe.
An example of training during this period (late 18th to the early decades of the 19th century) was that of John Ball Brown, who became the first physician in America to limit his practice to orthopaedic surgery. After apprenticeships with two different physicians in Salem, MA, he opened his practice in Dorchester in 1809. After practicing a few years, he began classes at Harvard Medical School and received a medical degree in 1813. His was a typical general practice of medicine and minor surgery until 1838, when at age 54, he opened the first orthopaedic hospital in the United States-the Orthopedique Infirmary at 8 Joy Street on Beacon Hill, Boston. Influenced by his two sons who had severe Potts disease, one of whom died, John Ball Brown limited his practice to the spine in his new infirmary.
Buckminster Brown, another son of John Ball Brown, survived Potts disease after eight years of bed rest. He graduated from Harvard Medical School in 1844. Influenced by his severe kyphoscoliosis and determined to practice only orthopaedic surgery, Buckminster Brown focused his postgraduate training overseas. He studied with Dr. William J. Little-first to describe spastic diplegia-at the Royal Orthopaedic Hospital in London; with Dr. Jules Guérin in Paris; and Dr. Louis Stromyer in Hanover, Germany. Buckminster learned how to do tendon releases in club feet, Achilles tenotomies (which Stromyer had performed on Little, who had an equinus deformity from polio contracted as a young child), new methods for treating congenital dislocation of the hip, Potts disease, scoliosis, rickets and other skeletal abnormalities. He also learned how to maintain correction of deformities after tenotomy with special apparatuses. After almost two years abroad, Buckminster returned to Boston in 1846 and became the first U.S. citizen trained in orthopaedic surgery. He practiced with his father at the infirmary and later became the chief orthopaedic surgeon at the House of the Good Samaritan in Boston.
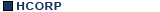
General adult and children’s hospitals began to be built in the U.S. in the early 19th century… in addition to almshouses for the poor which were established much earlier by the new settlers in America. In Boston, Harvard Medical School’s major teaching hospitals became:
- Massachusetts General Hospital (MGH): 1821
- Boston City Hospital: 1864
- Boston Children’s Hospital (BCH): 1869
- Peter Bent Brigham Hospital (PBBH): 1913
- Robert Breck Brigham Hospital (RBBH):1914
- Beth Israel Hospital (BIH): 1917
These hospitals quickly became the focus of graduate and postgraduate medical education in Boston.
As Harvard Medical School (HMS) increased its clinical teaching, students in the third and fourth year classes became “internes” at Massachusetts General Hospital (MGH) immediately upon opening (1821), at Boston City Hospital, immediately upon opening (1864), and at Boston Children’s Hospital (BCH) in 1882, 13 years after opening. HMS gradually increased the length of its curriculum from a few months at its founding in 1782 to two years, and then in 1871, to three years while Charles Eliot was president of Harvard College. In 1874, it adopted a four-year curriculum required for an M.D. degree.
“Internes” at MGH were soon assigned to assist the medical and surgical staff in addition to the custom of usual attendance at lectures and demonstrations.
As the hospital increased in size and added outpatient departments, the number of “internes” required for patient care also increased. By 1849 (28 years after opening), MGH began accepting some of the “internes” who were graduates of medical schools. As such, they often “assumed too much authority in care of patients”. Staff physicians at MGH, obviously upset, renamed the “internes” house pupils or “PUPS” which “more clearly defining their subordinate positions.” Junior residents at MGH and BCH were called “PUPS” for over 100 years…until some time during the last decade of the 20th century (exact date unknown).
Graduate medical education in the U.S. that began in the mid-and- latter part of the 19th century expanded rapidly in the first two decades of the 20th century. Graduates of medical schools now had the opportunity to further their education by accepting an internship in a hospital; they varied from six months to one year. For example, at Boston Children’s Hospital, surgical internships were six months. Interns could spend the entire time on surgery or choose three months on surgery and three months on a subspecialty such as orthopaedics or urology. Their primary responsibility was in the care of outpatients. At Massachusetts General Hospital, surgical internships were 12 months with opportunities for the interns to spend time on other surgical subspecialty services. All surgical internships were in the Department of Surgery at MGH and BCH. The number of surgical interns was small-usually one or two per year-but they gradually increased with time. An example of orthopaedic surgical training during the late 19th century was that of Dr. Joel E. Goldthwait. Dr. Goldthwait graduated from Harvard Medical School in 1889 and spent one year as a surgical intern at BCH (1890) followed by a second surgical internship at Boston City Hospital (1891). Influenced by Drs. E.H. Bradford and R.W. Lovett at both hospitals, Dr. Goldthwait limited his practice to orthopaedic surgery.
Orthopaedics became an independent department at Boston Children’s Hospital in 1903 (Table 1). However, all surgical interns remained in the Department of Surgery until 1914, when the house officers were separated into surgery and orthopaedic surgery. In 1914, the first resident in orthopaedic surgery was accepted into a one-year program at Children’s Hospital, while Dr. Robert Lovett was chief of the department. Dr. Frank Ober, who had graduated from Tufts, completed a one-year internship and practiced general medicine and surgery in Maine for seven years. He was the first resident in the future CH/MGH residency program.
At Massachusetts General Hospital, two orthopaedic House Pupils (“PUPS”) were added in 1909; previously the interns were on either the medical or surgical services. While on a surgical internship, a house officer would often have rotations on other surgical services, such as orthopaedics. One-year appointments as an orthopaedic house officer (intern) at MGH remained stable until after 1917 when they began to vary from three to seven per year. Some of the notable graduates of this one-year program included Drs. Charles Scudder, Marius Smith-Petersen, Mark Rogers, Zabdiel Adams, Philip D. Wilson, Sr., and George VanGorder.
In 1914, the American Medical Association (AMA) first conducted surveys (2424 hospitals in the U.S.) on the quality of hospital internships and published the first list of “approved internships.” The AMA selected a committee in each state to review every internship in that state and grade them for educational worth. Some of the requirements included general supervision of interns, the commitment of the hospital…to the community, to scientific medicine or solely for the profit of the attending staff…workload of the interns, educational progress and research influence on local physicians. In Massachusetts, for example, a committee of three was selected with Dr. Ernest Amory Codman, the father of the “end result idea,” as chairman. The surgeon’s education was now available in hospitals and no longer obtained in local apprenticeships. Since 1914, a one-year internship, in addition to four years of medical school, was required to obtain a license to practice medicine. In Boston, twelve-month internships were available at MGH, BCH, Boston City Hospital, Carney Hospital and the House of Good Samaritan.
The first published list of requirements for the training of an orthopaedic surgeon was published by the American Medical Association (AMA) in 1920. The minimum requirements in included:
- Graduation from a class A medical school (4 years)
- Completion of a surgical internship (1 year)
- Completion of a graduate course: “intern” on an orthopaedic service (1 year)
- Six months in allied studies: PT, shop work and schools for disabled children
Before these requirements in 1920, orthopaedic surgeons in the early 20th century in the United States completed a surgical or surgical and orthopaedic internship, or spent time abroad, and then limited, if possible, their practice to orthopaedic surgery. Common examples of individuals with this type of graduate training included these Harvard orthopaedic surgeons: Drs. E.H. Bradford, Arthur Legg, James Sever, Frederick Cotton, Alfred Ehrenfried, Joel E. Goldthwait, and Robert B. Osgood.
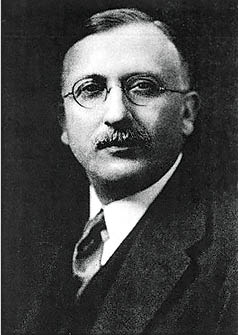
Robert B. Osgood, MD
By 1920, there was one resident per year at Children’s Hospital training in orthopaedic surgery and two to three orthopaedic house officers in a separate program at MGH. The first postdoctoral year continued to be called an internship, but additional training of house officers eventually became labeled a residency. In 1921, Dr. Lovett retired. At the request of the Dean, Dr. Osgood resigned as chief of orthopaedics at MGH and became the chief of orthopaedics at Boston Children’s Hospital and the John Ball and Buckminster Brown Professor at Harvard Medical School. He was succeeded at MGH by Dr. Nathaniel Allison. The timing was perfect for combining the orthopaedic training programs at Children’s Hospital and MGH. “This department [orthopaedics at Children’s Hospital], formed a gentleman’s agreement with the Orthopaedic Staff of the MGH, giving the House Officers a Combined Service” (F. Ober, 1935). Dr. Osgood “was able to arrange the incorporation of the resident training programs of the MGH and Boston Children’s Hospital into a single program under the aegis of HMS.” (Philip Wilson, 1952). It was Dr. Osgood’s goal to have orthopaedic residents train in both children’s and adult orthopaedics; including fracture care, which was possible at the MGH. As Thornton Brown would later write, “the Combined Residency Program, as we know it today, emanated from the Children’s engineered by the deft diplomacy of Robert Bayley Osgood” (Robert Osgood Lecture, early 1990s).
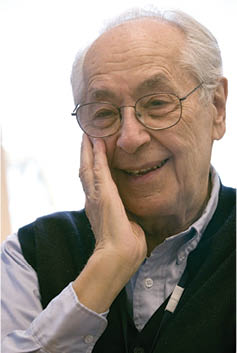
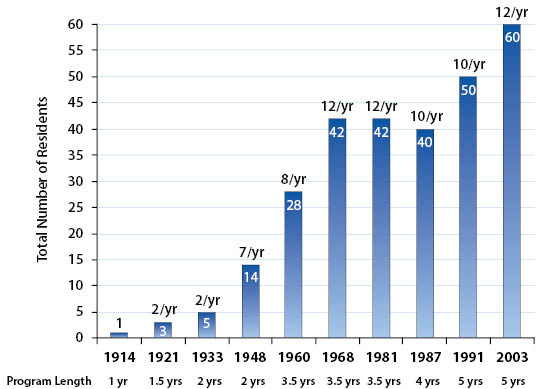
Thus in 1921, the combined orthopaedic residency program at Harvard began under the auspices of the Harvard Medical School for Graduates (HMSG). The program was 18 months in length for two residents per year; with six months at Harvard studying “fundamentals” (basic science), six months at Children’s Hospital and six months at the MGH (adult and fractures). The orthopaedic residents were required to complete “a previous experience in general surgery.” Later, at an unknown date, the administrator for the combined program was transferred to MGH. The first residency director for the new combined program was Dr. Robert B. Osgood (Figure 1).

Dr. Osgood was an “interne” at the House of the Good Samaritan during his fourth year at HMS. After graduation in 1900, he was a surgical house officer at MGH. Fascinated by x-rays and working with Walter J. Dodd-apothecary and photographer at MGH, Osgood accepted his first job at Children’s Hospital as its second skiagrapher (radiologist) following E. Amory Codman. It was while he worked at Children’s (1901-1903) that Osgood described lesions of the tibial tubercule which bear his name. In 1903, he went to Europe for additional training in orthopaedics. After returning to Boston, he joined the staff at MGH and in 1917 collaborated with Dr. Charles L. Scudder in establishing the first fracture clinic. During, and after WWI, Osgood joined Dr. Goldthwait and others to lead the movement to include fracture care within orthopaedic surgery. Dr. Osgood emphasized teaching and research in the residency program. He began a monthly (Sunday morning) end-result clinic (following his colleague’s, Dr. Codman’s teaching), and started specialty clinics-always emphasizing patient safety.
Frank R. Ober, MD
The second program director was Dr. Frank R. Ober (Figure 2). His initial action as head of the residency program in 1930 was to increase its length to two years…an eight month rotation at Children’s Hospital, an eight month rotation at MGH and an eight month rotation at a chronic hospital which included a laboratory experience at HMS. In 1933, Ober-Assistant Dean, HMS for Graduate Courses-chaired a committee of the American Orthopaedic Association (AOA) to study the status of orthopaedic residencies in the U.S. The committee reported that only 15 of 62 medical schools had an orthopaedic department and there were few, if any, similarities in any of the residency programs. He reported that Harvard’s two-year orthopaedic residency program required one year of surgery or two years of a rotating internship before entering the program. Dr. Ober also noted that there was a chief resident on each of the services in the Harvard residency whose main responsibility was teaching. He described the HMS for Graduate Courses in orthopaedic surgery as “the most completely organized” course. In addition to receiving clinical instruction by the staff, the residents were “allowed to do operations assisted by the staff on service and took care of patients in the wards under the direction of the visiting surgeons and are held responsible for their care.”
In 1934, 20 years after the AMA published its first list of approved internships, the AMA’s newly formed Council on Medical Education and Hospitals published the first list of approved residencies in specialties in the United States. House officers were now clearly labeled as interns or residents during their hospital postgraduate training/education. In this publication, there were 44 approved orthopaedic residency programs in the U.S.-three in Boston. The three hospitals approved for orthopaedic residents in Boston included Children’s Hospital, MGH and Boston City Hospital. Nineteen thirty-four was also a significant year because this list of approved residencies established the process of accreditation of individual programs. Standards had to be met in order for the program to be approved. Also in 1934, the American Board of Orthopaedic Surgery was formed (after Ober’s report). The first certifying examination (individual certification) was given in 1935. It consisted of four essay questions. Residency programs were now being accredited and individual orthopaedic surgeons who successfully passed their board examinations were listed as certified.
The American Board of Orthopaedic Surgery (ABOS) developed requirements needed for an individual to be eligible to take the certifying examination in 1935. Ober immediately changed the Harvard program to meet these requirements by lengthening the clinical rotations to one year (one year at Children’s Hospital and one year at MGH) and requiring that each resident complete eight months of pathology before starting the clinical rotations. In 1944, Ober again increased the length of the program to three years. The one-year rotations at Children’s Hospital and MGH continued, but the eight months of pathology was reduced to six months, and he added six months of training in fracture management to meet new ABOS requirements. Frequently, the program was referred to as “combined,” “coordinated,” or “integrated.”
William T. Green, MD
Dr. William T. Green (“WTG”), who graduated from the University of Indiana School of Medicine, interned and began his orthopaedic training at Henry Ford Hospital in Detroit. He then moved to Boston for one year as a resident in surgery at the Peter Bent Brigham Hospital (PBBH) followed by a year of orthopaedic residency at Children’s Hospital. He was Dr. Ober’s first resident in 1930. Dr. Green was a strong advocate for teaching (as all HCORP directors have been). He advocated that 20-25% of a medical school’s curriculum be devoted to orthopaedics; a goal he never achieved. He didn’t believe in many lectures during residency education but emphasized hard work (“residents were worked to exhaustion”) and that supervised care was the best way to teach.
Dr. Green made many changes in the program while serving as the third residency program director (Figure 3). In 1948, he increased the residents to seven per year (total: 14). Residents started the program at three-month intervals. In 1960, Dr. Green added another resident in the starting class (now 8 per year; total: 28) and increased the length of the program to three and a half years. In 1962, Chief Residents (for six months at the end of residency) were assigned to the following hospitals: Children’s Hospital, MGH, Peter Bent Brigham Hospital (PBBH) and the West Roxbury Veterans Administration Hospital (WRVAH). In 1963, residents at Children’s Hospital began a three month rotation at the newly affiliated Robert Bent Brigham Hospital (RBBH). The prerequisite internship plus one year of surgical residency remained in place.

Dr. Green held weekly “prayer” meetings with the residents; so-called because for years they were held on Sunday mornings after making rounds with the staff and residents at both BCH and the PBBH. He believed strongly in having “several visiting men who have periods on house service and office service. This gives diversity to the teaching program, but continuity must be maintained by the orthopaedic surgeon-in-chief. Outpatient clinics should be attended by visiting men who consult and advise. The major activities of the clinics, however, should be performed by the resident staff…The men in training must do the work; observation has limited value. The teaching of surgery must be well supervised. Training should evolve through assisting, performing operative procedures assisted by a competent teacher, with progression to more independence as a senior resident. A man cannot learn surgery unless he does it… ‘Resident rounds,’ including the visiting staff and residents, should be made daily with all residents in attendance…Ideally each resident should have a research project for investigation and report.”
The Residency Review Committee (RRC) for Orthopaedic Surgery was formed in 1955. As with other specialty RRCs, it was charged with establishing the educational and training standards for all orthopaedic residency programs. Initially reporting to the AMA and the ABOS, it became a tripartite committee reporting to the AMA, the ABOS and the American Academy of Orthopaedic Surgeons (AAOS) in 1973. It consists of nine members, three from each of the parent organizations, and one resident member. Since 1981, all RRCs have been part of the Accreditation Council for Graduate Medical Education (ACGME) and have a high degree of autonomy.
Melvin J. Glimcher, MD
The fourth program director was Dr. Melvin J. Glimcher (Figure 4). After graduating from HMS and completing a surgical internship at Strong Memorial Hospital in Rochester, NY, he was an assistant resident in surgery at MGH and completed his orthopaedic training in the Children’s Hospital/MGH combined program. A basic scientist at both the MGH and MIT, he opened the first orthopaedic research laboratory at MGH with the support of Dr. Joseph Barr-chief of orthopaedics at the time. In 1968, the number of residents in the program was increased to 12 per year; three starting every three months. The program included: first nine months at Children’s Hospital (ABOS reduced the children’s requirements to six months in 1971), next fifteen months at the MGH, followed by a second six month rotation at Children’s Hospital. Residents rotated for the next six months at two of six affiliated hospitals (RBBH, PBBH, WRVAH, BIH, Lemuel Shattuck Hospital or Lynn Hospital). During their last six months, they served as chief resident at one selected hospital. Many residents spent three to twelve months in the laboratory after their surgical training and before entering the clinical orthopaedic program. The total number of residents on clinical services was 42. In 1970, Dr. Glimcher authorized a required rotation for residents at Beth Israel Hospital (BIH) with the assistance of Dr. Seymour (“Zeke”) Zimbler and Dr. Harris Yett.
Henry J. Mankin, MD
In 1972, Dr. Henry J. Mankin became the fifth MGH/BCH residency program director (Figure 5). A graduate of the University of Pittsburgh School of Medicine and its orthopaedic residency program, he had completed his internship and one year of surgical residency at the University of Chicago. Prior to being recruited to Boston as chief of the Orthopaedic Department at MGH, he was the chief of orthopaedics at the Hospital for Joint Diseases in New York City for six years. Dr. Mankin would only accepted his new position at MGH if also named the orthopaedic residency program director, because like his predecessors, he was dedicated to education. Sometime between 1972 and 1976, he, along with Dr. Clement Sledge (chief at RBBH and PBBH) and Dr. John Hall (chief at Children’s Hospital) formed the Harvard Orthopaedic Executive Committee and named the residency program the Harvard Combined Orthopaedic Residency Program, or “HCORP.”

Dr. Mankin made many significant changes in the program. Some of the major ones included: daily breakfast meetings with the residents, initiation of the annual Osgood Lecture, mandatory thesis requirement for all graduating residents, organization of the the first Boston Pathology Course with Dr. Crawford Campbell, and, in 1984, implementation of a core curriculum. In 1972, the program length remained at three and a half years after preliminary training in surgery. Two tracts of resident rotations were started…the MGH-CH-BIH tract and the Brigham (RBBH/PBBH)-CH-BIH tract. A significant change occurred in 1980 when Dr. Mankin wrote, “We were the first to privatize the ward services in an attempt to establish one class of care.” Each chief resident was now given a new status. No longer included in the ACGME-approved residency program (ABOS), each graduating resident was now required to spend an additional six months as an “assistant in orthopaedics” and given admitting and surgical privileges to care for ward cases in the clinics, the operating room, and in the emergency department. Paid a small salary, they required only “minimal supervision.” The program was effectively lengthened to four years (three and a half years plus six months as chief resident). Half of the residents also spent six months in the laboratory.
James H. Herndon, MD, MBA
Two years later, the Partners leadership and Dean Joseph Martin recruited Dr. James Herndon as the inaugural Partners Professor and Chairman of the Partners Department of Orthopaedic Surgery (Figure 6). He graduated from UCLA Medical School, completed a rotating internship and a year as a surgical resident at the Hospital of the University of Pennsylvania, and graduated from the MGH/BCH combined orthopaedic program in 1970. For two decades prior to assuming his Partner’s chair, he had been Chairman and Resident Program Director at both Brown University and the University of Pittsburgh. Following Dr. Mankin’s lead, Herndon accepted the position with the understanding that he would also be the sixth residency program director. Herndon also rejected the planned reduction in the size of the residency program, and Partners agreed to maintain the total number of residents at 50 in the five-year program. In 2003, he increased the number of residents per year from 10 to 12 (total: 60 in the program) with both Partners and ACGME approval (Figure 7).
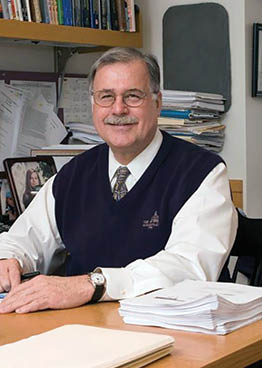
Other milestones achieved while Dr. Herndon was Program Director included: a new core curriculum developed in 1998 which, for the first time, included cadaver dissections on Wednesdays (half day) at HMS in July and August. Six cadavers were purchased yearly. Initially, Dr. Richard Ozuna oversaw the program of planned regional dissections by the residents with an examination at the completion of the course. Dr. Ozuna was later replaced by Dr. Scott Martin who has been responsible for the anatomy program for more than 10 years. Two weekly Grand Rounds (Wednesday at the BWH; Thursday at the MGH) were combined into one: 7 a.m. Wednesday Grand Rounds were held at the MGH the first two Wednesdays of the month and at the Brigham and Women’s Hospital (BWH) the second two Wednesdays. They alternated on the occasional fifth week. The Core Curriculum was held immediately following Grand Rounds at the same hospital for four hours (8-12 p.m.) each Wednesday. For the first time, all residents from all the affiliated hospitals assembled together in this major, required, and protected teaching commitment by the faculty. Weekly Saturday breakfast meetings with the residents were held by the Program Director. Routine orthopaedic cases were not discussed. Instead, Dr. Herndon developed a curriculum for discussions consisting of such topics as reimbursement issues (Medicare and Medicaid), coding fundamentals, employment contracts, private versus academic practice, the Balanced Budget Act (RBRVS and RVUs), medical errors and patient safety, ethics, physician-hospital relationships (specialty hospitals; ASCs), malpractice, financial planning, disparities, gainsharing and pay for performance for both academic and private practicing physicians.
Faculty/resident retreats were started, and the Orthopaedic Journal at Harvard Medical School was initiated by Dr. Herndon in 1999. He used the model of the resident journal that he began at the University of Pittsburgh: a yearly journal produced entirely by the residents selected from each class who became editors in their senior year, and were mentored by selected staff. The purpose of the journal was to inform the Harvard orthopaedic family (residents, faculty, fellows and alumni) and resident applicants about the current status of the residency program, provide updates on developments in each hospital’s orthopaedic departments (Chiefs’ reports), introduce new residents, recognize the year’s graduates, and to publish some of the interesting clinical and laboratory research in each hospital and HMS…as well as provide the unique educational experience of producing a journal (peer reviewed) by the residents. In 2000, Steve Nestler, Executive Director of the Orthopaedic RRC, wrote, “The Committee commended…[the] teaching staff for the steps that have been taken to establish one, integrated Harvard program and improve the structure and organization of resident education.”
In 2003, with the support of the residents and the executive committee, Dr. Herndon discontinued the required additional six months of “chief residency” and restored the total program length to five years, which included a period of time in their last year (PGY5) to be named chief resident. During 2002 and 2003, the ACGME required education in six core competencies (“Outcome Project”) and mandated the 80 hours per week work rules. HCORP complied with all these changes, including for example…starting a night float system. The hospitals’ department chiefs aided the residents’ burden in patient care and administrative tasks by hiring physician extenders (NPs and RNs) at each hospital.
Dempsey S. Springfield, MD
Dr. Dempsey Springfield became the seventh Program Director upon Dr. Herndon’s retirement in December, 2008 (Figure 8). He graduated from the University of Florida College of Medicine and trained in orthopaedics at the University of Florida Health Shands Hospital. After being a member of the orthopaedic tumor service at MGH for a number of years, he was appointed Chief of Orthopaedics at Mount Sinai Medical Center in New York City. Eventually, he returned to MGH. When he assumed the directorship of HCORP, the PGY1 rotations had become unacceptable. Rotations assigned by the surgery residency program director to HCORP residents, similar to other surgical specialties’ residents, were selected essentially for service requirements. Education was not the primary goal. As such, many of these rotations were on surgery’s unpopular services. Dr. Springfield developed a rotation schedule for all PGY1 orthopaedic residents at the MGH, BWH and BIDMC that were educationally important to the residents and met the ABOS requirements. He obtained approval for the specific rotations from each of the parent departments and controlled the entire PGY1 year, in addition to the four years of orthopaedic rotations.

George S. M. Dyer, MD
The eighth and current HCORP Director is Dr. George Dyer (Figure 9). Dr. Dyer is a graduate of HMS and HCORP and was appointed to his position in 2012. He is responsible for the following milestones: initiatng a “Boot Camp” for all PGY1 residents. It consists of four weeks of intensive training with simulation for basic technical and nontechnical skills required of orthopaedic surgeons. Within the ABOS guidelines, he developed flexible rotation schedules in which the PGY4 and PGY5 residents can select a large portion of their rotations which meet their individual specific interests. With the residents’ participation, six Orthopaedic Societies were formed, each consisting of two residents per year, led by two faculty advisors. Their purpose is to build camaraderie and mentoring. Each society was named for a famous former Harvard faculty member: Otto E. Aufranc, E. Amory Codman, Robert B. Lovett, Thomas B. Quigley, Marius M. Smith-Petersen and Augustus White. He also incorporated the ACGME “Milestones Project” into the residency program.

Dr. Dyer’s latest contribution has been the organization of HCORP’s Annual Alumni Day. The first was held in Boston, at MGH on October 21, 2017. After Dr. Dyer’s welcoming comments, Dr. Herndon gave the keynote address, “Historical Perspective: First 100 Years of HCORP. Selected Contributions by Harvard Orthopaedists…Famous and Not So Famous.” The attendees then heard from three recent HCORP graduates about their experiences in practice today-Dr. Joseph J. Czarnecki, R’04, Dr. James D. O’Holleran, R’03, and Dr. Boyan Zoric, R’07. At a Town Hall and lunch sessions, Dr. Thomas J. Gill, R’96 and Dr. Olivia C. Lee, R’11 led a discussion on “The HCORP Alumni Association of the Future.” Dr. Dyer concluded the day by encouraging all alumni to support and participate yearly in this major new initiative.
Remember…2021 will be the 100th Anniversary of the Harvard Combined Orthopaedic Residency Program (HCORP).