Childhood Obesity: Adverse Effects on Activity and Hip Range of Motion
Benjamin J. Shore, MD, MPH, FRCSC, Benjamin Allar, BA, Patricia E. Miller, MS, Yi-Meng Yen, MD, PhD, Travis H. Matheney, MD, MLA, Young-Jo Kim, MD, PhD
The authors report no conflict of interest related to this work.
©2018 by The Orthopaedic Journal at Harvard Medical School
BACKGROUND This study investigated the adverse effects of childhood obesity on hip range of motion (ROM) and activity. We hypothesized that the presence of obesity at an earlier age, for greater duration, correlates with decreased hip ROM and activity compared to ideal weight controls.
METHODS A prospective cross-sectional study of 100 children was performed. We defined children as either ideal weight (BMI>5th percentile - <75th percentile) or obese (BMI≥95th percentile, >1 year). Children under 14 years of age without underlying lower extremity injury, musculoskeletal or systemic conditions were included. Standardized hip ROM measurements were recorded for each hip separately and all subjects completed a UCLA activity score at their ROM recording. Measurements were compared across stratified age and weight groups using unbalanced two-way analysis of variance (ANOVA) via general linear modeling (GLM) with an interaction effect for age group * weight group. Pearson’s correlation analysis investigated the relationships between age, obesity, and ROM.
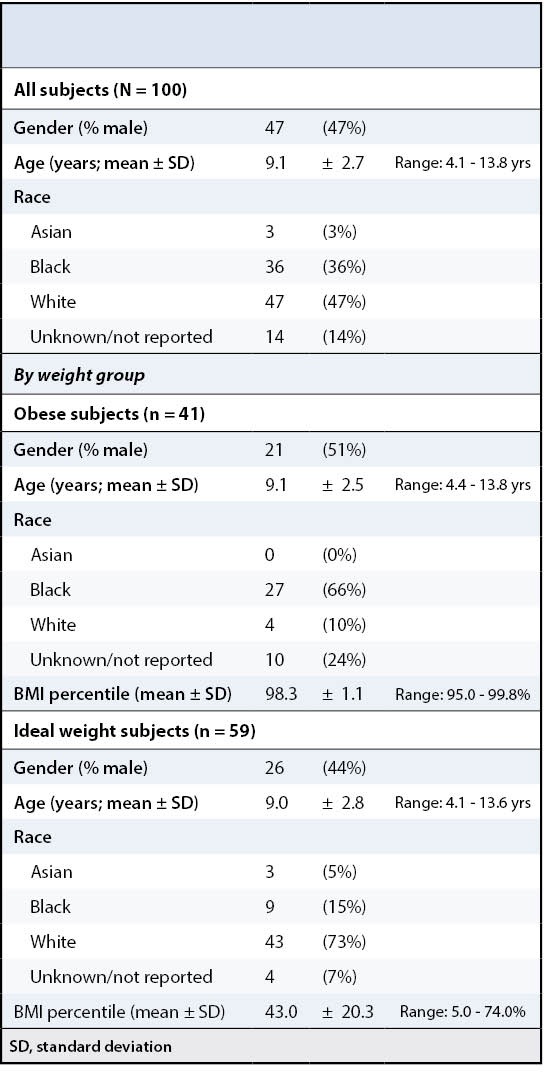
RESULTS Two hundred hips in 100 patients (47 male and 53 female) were measured at a mean age of 9.1 years (range, 4.1 to 13.8 years). Fifty-nine ideal weight children (BMI 43% +20.3) and forty-one obese children (BMI 98.3% +1.1) were measured. Significant differences across weight groups were seen in all ROM measurements (p ≤ 0.001) except external rotation (in flexion and extension) and abduction in extension. Obese children were less active than ideal weight controls (UCLA score = 7 versus 10, p < 0.001). Subgroup analysis in older subjects (>8 years) determined that internal rotation in flexion was significantly lower for obese subjects compared to the ideal weight group (30.4° ± 7.3 and 40.5° ± 8.8, respectively; p < 0.001).
CONCLUSION Obese children demonstrate significant differences in activity and hip range of motion compared to ideal weight children. A dose dependent effect may exist, where children who experience obesity at a young age experience the greatest deviation from normal.
LEVEL OF EVIDENCE Level II Prognostic
KEYWORDSObesity, femoral retroversion, UCLA activity score, slipped capital femoral epiphysis
Over the past twenty years, childhood obesity has more than doubled in children and quadrupled in adolescents.1,2 Obesity is a serious public health problem in children as well as adolescents and is the most prevalent nutritional problem for children in the United States.3 Some orthopaedic disorders that are unique to childhood also have been suggested to be weight related. Retrospective analyses of children with slipped capital femoral epiphysis (SCFE) and adolescent tibia vara (Blount’s disease) reveal overrepresentation of overweight individuals.4 Few prospective studies exist that quantify the prevalence and manifestations of potentially-weight related orthopaedic conditions in overweight children and adolescents.
SCFE is the most common hip disorder of adolescence, with prevalence as high as 10.08 per 100,000 observed in the northeastern United States.5 The etiology of SCFE is thought to be multifactorial. As the incidence of childhood obesity has increased, so too has the incidence of SCFE. SCFE is occurring in greater overall numbers,6,7 in children at increasingly younger ages,7 and in the form of bilateral SCFE to a greater degree than previously reported.8-10 Decreased femoral anteversion is another predisposing factor believed to be associated with SCFE and has also been reported in higher incidence in children with SCFE.11 Limited prospective studies, however, have investigated the changes in proximal femoral anatomy in obese children and adolescents who are asymptomatic in terms of hip symptoms and known pathology.
The purpose of this study was to investigate the adverse effects of childhood obesity on hip range of motion and activity compared to age-matched, ideal weight children. Our hypothesis was that the effect of obesity on hip range of motion and activity is dose and age dependent, such that obesity when present at an earlier age and for a greater duration correlates with a greater alteration in range of motion and activity compared to ideal weight controls.
After institutional board review, we performed a single hospital, prospective cross-sectional study examining hip range of motion and activity in children, divided into two groups based on body mass index (BMI, Ideal and Obese weight groups). Ideal weight children were defined as those children with a BMI between 5-75th percentile for the previous two years, while obese children had a documented BMI over the 95th percentile for greater than one year. Each group of children was further stratified into two chronologic age groups (4-8 and 9-13 years), based on previous biomechanical studies on shear stress on the hip.12--14 Children were recruited from the urgent orthopaedic and primary care clinics. Children with an underlying musculoskeletal condition, history of lower extremity injury (including previous slipped hip), or other systemic diagnoses capable of affecting lower extremity range of motion were excluded from the study. Informed consent was obtained for all included patients.
For each patient, hip range of motion (ROM) measurements were performed with a goniometer using a standard technique previously described by Sankar et al.15 by one of two authors (BJS, BA). Abduction, adduction, hip flexion, internal rotation in flexion, and external rotation in flexion were all recorded in the supine position for both right and left hips. Extension, internal rotation, and external rotation were recorded in the prone position for both right and left hips. In addition, arcs of motion (combination of internal and external rotation) in both flexion and extension were calculated for each hip. Radiographic hip examination was not part of the clinical examination, and during the study period no patients experienced a SCFE.
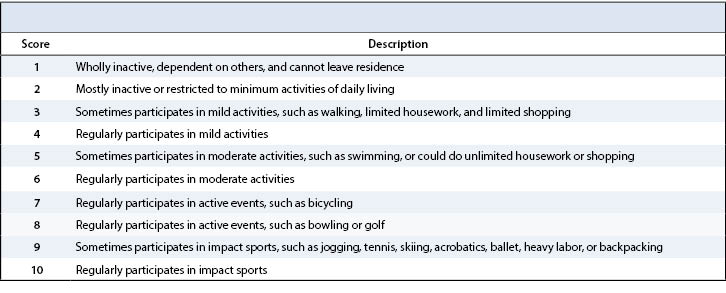
All patients completed a University of California at Los Angeles (UCLA) activity score at the time of ROM measurement, in children who were unable to complete the score it was completed by their parent (Table 1). The UCLA activity score is a 10-point clinician or self-reported questionnaire used to quantify activity and function. The UCLA score has been found to be an accurate assessment tool for global function and a reliable tool for monitoring physical activity and function in large populations.16 While initially developed as an adult assessment instrument, it has accurately been applied in the pediatric population.17-19
All ROM measurements, including arcs of motion, were summarized across weight and age groups by means and standard deviations. Measurements were compared across stratified age and weight groups using generalized linear modeling (GLM) with a general estimating equations (GEE) approach. For each ROM measurement, an individual model including interaction effect for age group * weight group was developed and analyzed to assess the effects of age and weight on each measurement. Recognizing the correlation between recording both the right and left hip ROM measurements for each subject, we employed the GEE approach to control for potential correlation between bilateral measurements on the same subjects. ROM data were complete for all subjects and no deviations from normality nor GLM assumptions were detected. UCLA scores were summarized by median and interquartile range (25th to 75th percentile) due to deviation from the normal distribution. UCLA scores were analyzed using a non-parametric Kruskal-Wallis test for age and weight group effects. Correlation between ROM measurements and patient age at time of study, age at onset of obesity, as well as duration of obesity was analyzed using Pearson’s correlation analysis. Duration of obesity was defined as the amount of time over the 95th percentile limit based on existing hospital records. Subgroup analysis was conducted to assess the effect of age on ROM measurements in the obese subgroup and to compare ROM in older subjects across weight groups. All tests were two-sided and p-values less than 0.05 were considered significant.
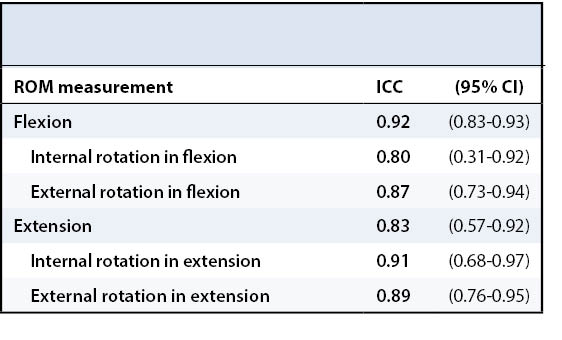
A random sample of 25 patients from the original cohort was selected to test the reliability of the physical examination. Two of the authors (BJS, BA) performed independent recordings on these 25 patients to test interrater reliability using Intraclass Correlation Coefficients (ICC) with 95% confidence intervals. Strength of agreement was defined <0.4 as poor, 0.4-0.75 fair to good and >0.75 excellent.20 Raters demonstrated excellent agreement with the ICC ranging from 0.80-0.92 (Table 2).
Two hundred hips were measured in 100 patients (47 male and 53 female). The mean age of study participants was 9.1 years (range 4.1 to 13.8 years). The obese group contained 41 children with a mean BMI percentile of 98.3 (+1.1) and the ideal weight group contained 59 children with a mean BMI percentile of 43.0 (+20.3). There were no significant differences between the two groups in terms of age or gender; however, the ideal weight group was composed predominantly of Caucasian subjects (73%), while the obese group was composed of predominantly African-American subjects (66%) (Table 3). No significant differences between right and left hips were detected for any measurement as a group or as individual patients. Mean and standard deviation of hip ROM measurements are reported for all 200 hips in Table 4.
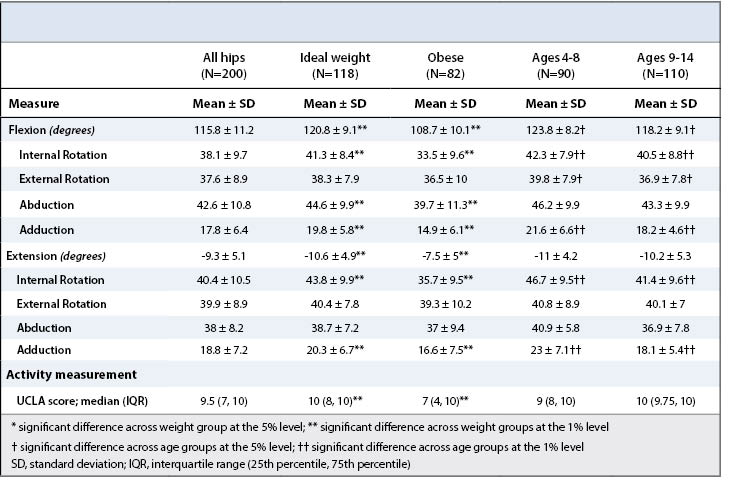
Significant differences across weight groups were seen in all ROM measurements (p ≤ 0.001) except external rotation (in flexion and extension) and abduction in extension (Table 4). Furthermore, the distribution of activity scores was significantly lower in the obese weight group [median 7, IQR (4-10)] compared to the ideal weight group [10, (8-10)] based on the UCLA activity scores (p < 0.001) (Table 4). There was a significant difference in arc of motion across weight groups in extension (p < 0.001) and in flexion (p < 0.001) (Table 5). Age was negatively correlated with both the arc of motion in flexion (r = -0.30, p < 0.001) and extension (r = -0.32, p < 0.001). Looking at younger subjects, there was a significant difference in arc of motion in extension across weight groups (p = 0.02) but not in flexion (p = 0.13). In the older age group, however, a significant difference in arc of motion was recorded for both flexion (p < 0.001) and extension (p = 0.01). There was no difference detected in activity level across age groups (p = 0.20). Multivariable analysis determined that the effect of weight group was independent of the effect of age group and vice versa for all ROM measurements.
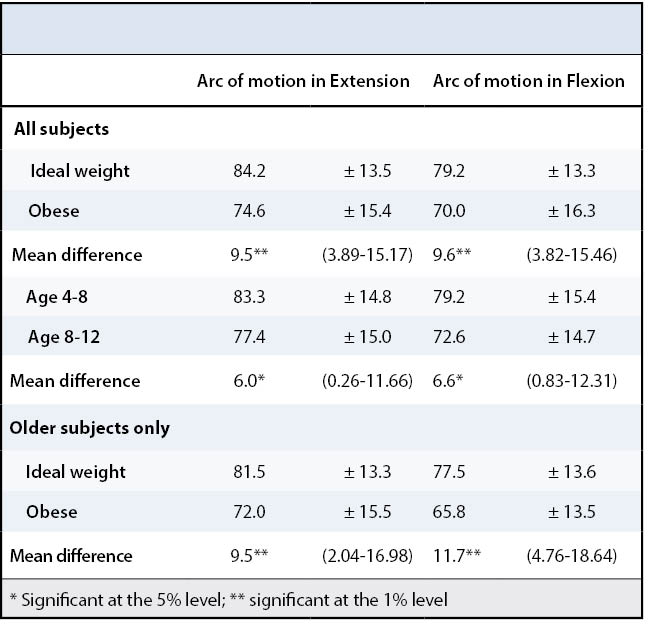
Although the differences in most ROM measurements were negligible across age groups, there was a significant relationship between subject age and internal rotation in flexion. Age at the time of study was negatively correlated with internal rotation in flexion (r = -0.24; p = 0.02). In addition, subgroup analysis looking at only older subjects determined that internal rotation in flexion was significantly lower for obese subjects compared to the ideal weight group (30.4° ± 7.2 and 40.5° ± 8.8, respectively; p < 0.001). Not surprisingly, patient age at time of study was positively correlated with duration of obesity (r = 0.40; p = 0.009). However, duration of obesity as measured by the clinical record was not correlated with internal rotation in flexion (p = 0.24), according to our sampling of the medical record to assess for duration of obesity.
Obesity is a tremendous public health problem in the United States and the epidemic of childhood obesity has led to the recognition of obesity-related childhood and adolescent morbidities such as diabetes, hypertension, cardiovascular disease and musculoskeletal comorbidities.21-27 This epidemic has led to a near-doubling in hospitalizations with a diagnosis of obesity between 1999 and 2005 and an increase in costs from $125.9 million to $237.6 million between 2001 and 2005.16 Obese children report more frequent as well as more severe joint pain and lower extremity mal-alignment is more prevalent in obese children.1,29-33 Despite our understanding of the general risks associated with childhood obesity, there have been limited prospective studies in asymptomatic obese children. This study demonstrates that obese children experience significant alterations in hip range of motion and activity level compared to ideal weight controls. Furthermore, preliminary results suggest that a dose dependent effect may exist, where children who experience obesity at a younger age and for a longer duration may likely experience the greatest range of motion deviations from normal.
Slipped capital femoral epiphysis (SCFE) is characterized by displacement of the capital femoral epiphysis from the metaphysis through the physis. While the exact etiology of SCFE is unknown, it is thought most commonly to be a combination of biomechanical and biochemical factors including obesity, increased femoral retroversion, pituitary axis disorders, and endocrinopathies.34 It has been widely accepted to be a disease of the obese adolescent.35 The association of SCFE and obesity has been found in several countries, including the United States.36 In 2005, Manoff investigated the correlation between BMI and SCFE and found that for those with SCFE, 81% had a BMI percentile over 95%.35 Benson et al.37 reported a doubling of the rate of SCFE in New Mexico between 1960 and 2008 and noted that the rate of obesity in their area had tripled since 1971. A similar trend was demonstrated in Scotland, where the incidence of SCFE increased from 3.78 per 100,000 children in 1981 to 9.66 per 100,000 children in 2000, representing a 2.5 increase over 2 decades.7 More recently, Nasreddine et al.38 found that persistent obesity after initial slip increased the chances of contralateral slippage by 3.5 times compared to children who were able to obtain and maintain a normal BMI. However, the mechanism of this increased risk of SCFE among obese children and adolescents has not been clarified prospectively.
In 1953, Dunlap et al.39 suggested that reduced femoral anteversion might increase the stress on the epiphyseal plate and lead to a SCFE. Although conceptually sound, there has been limited further research to support this assertion. Gelberman et al.40 examined 25 patients with SCFE and determined the degree of anteversion in 39 hips via computed tomography. Only 13 of these patients had their examination at the time of presentation, the remaining had their examination between one and seven years post SCFE. The authors found a mean anteversion for all SCFE hips of 1.0° +8° compared to 6.3° +8.2° for the unaffected side. While it is clear that femoral retroversion may be associated with SCFE, there is no evidence to suggest a cause and effect. Studying a small sample of 25 children, Galbraith et al.41 found an average angle of femoral anteversion of 10.6° (SD of 8.6°) in ideal weight children and 0.40° (SD of 13.0°) in obese children. To our knowledge, our study is the first prospective investigation in asymptomatic patients with obesity, attempting to measure and compare femoral rotation.
A variety of assessment techniques have been described for the measurement of femoral rotation including physical exam maneuvers, static biplanar radiography, fluoroscopy, two and three-dimensional computed tomography (CT)/ Magnetic Resonance Imaging (MRI) and ultrasound.42 Cross-sectional imaging scanning is widely considered the most accurate method for the quantitative assessment of femoral anteversion in children.42 However, there is less consensus for measurement of femoral retroversion. Botser et al.43 compared the correlation between CT, MRI and physical examination measurements for femoral anteversion. The authors found a significant correlation between internal rotation determined by clinical exam and anteversion calculated by CT scan (r=0.36, P < 0.001). In our study, we found that obese children experienced significant differences in all ranges of hip motion except external rotation. If we extrapolate what we know from the correlation between internal rotation and anteversion, one can assume that this preservation of hip external rotation correlates with increased femoral retroversion in the obese group or a loss of femoral anteversion. However, further three-dimensional imaging studies on this population are needed to establish the proposed correlations between obesity and femoral retroversion.
Biomechanical forces have been shown to contribute specifically to the regression of femoral anteversion associated with normal growth. Growing bone is a dynamic tissue that responds to the mechanical stresses and loads placed on it. The Hueter-Volkman law states that bone growth is suppressed by an additional compressive loading through the immature growth plate and that growth is accelerated by tensile forces across the growth plate.44 In unaffected gait, the resultant force across the femoral head is 6.5 times body weight,13 while in obese children every kilogram of weight gained magnifies the shear force acting on the femoral head by a factor of 4 to 10, depending on activity.45,46 Cadaveric studies have demonstrated that the forces necessary to cause displacement of the epiphysis in the immature human skeleton are within the range of the force that can be generated in overweight children.13 Therefore, mild malalignments in the lower extremity coupled with additional forces caused by excessive weight secondary to obesity have the potential to cause proximal femoral deformity at the physis. This repetitive microtrauma leads to progressive growth plate dysfunction that exacerbates the deformity and establishes a vicious cycle for the development of SCFE.47,48 Although identifying a relationship between SCFE and obesity is beyond the scope of this prospective study, we have demonstrated that in asymptomatic obese children there is an increase in hip external rotation and a decrease in hip internal rotation, which appears to be age and duration/dose dependent. We believe this is the first project to prospectively quantify changes in hip motion related to age of onset of obesity.
This study is not without limitations. There were higher proportions of Caucasian and African-American children in the ideal and obese weight groups, respectively. This inequality represents the challenges associated with prospectively recruiting obese children. We have not been able to identify any studies that highlight significant differences in lower extremity range-of-motion among races. Our inclusion criteria required documented obesity for greater than one year or ideal weight for greater than two years, which made it challenging to recruit subjects due to sparse medical records for otherwise qualified participants, which may have introduced some degree of selection bias. Furthermore, we relied on the medical record to determine the duration of obesity. While we recognize that the duration of obesity may be underestimated by using the medical record, all included obese patients had been longitudinally followed in our primary care clinic, we believe that the calculated duration of obesity was accurate to within 12 months. Despite this limitation, we believe the duration of obesity information that we have collected in this study is of clinical value to the reader. While we have demonstrated a negative association between obesity and hip range of motion, it is possible that the observed decrease arc of motion could be as a result of a protuberant abdomen or pannus rather than a true alteration in proximal hip morphology. Finally, as with any range-of-motion study, there is no ability to differentiate the effects of bony versus soft tissue limits on hip range of motion and obesity and size of the abdomen could have impacted on our clinical measurements. Without three-dimensional imaging, we can only make assumptions about the bone structure, which is why further imaging studies on this population are needed.
While previous authors have demonstrated a correlation with femoral anteversion and hip internal rotation,43,,ass="sup">49 this has yet to be proven for femoral retroversion. Therefore, the second stage of this study will be to correlate the degree of rotation observed in our typical and obese cohorts with three-dimensional MRI of the proximal and distal femur to calculate true femoral retroversion angles. We recognize that a lack of three-dimensional imaging is a weakness of this study, but to justify this expensive imaging modality in asymptomatic children we felt necessary to first demonstrate that a true difference in hip motion and activity existed between these two cohorts to justify further study.
In conclusion, this prospective cross-sectional study has demonstrated several important findings. Children with documented obesity (BMI>95% for over 1 year) demonstrate significant alterations in activity levels and hip range of motion compared to unaffected ideal weight children. These changes in activity and range of motion appear to be related to age of onset of obesity and duration of obesity, suggesting that early recognition of an “at-risk” child is paramount. Further prospective studies investigating the three-dimensional changes occurring at the proximal femur in obese asymptomatic children will aide physicians in stratifying children at risk for slipped capital femoral epiphysis and other orthopaedic conditions.