Current Research at the MGH Orthopaedic Hand Surgery Service: New Technologies for the Treatment of Trauma Sequelae in the Elderly patient
Santiago A. Lozano-Calderón, MD; Jess e B. Jupiter, MD
Massachusetts General Hospital
Introduction
The use and development of new technologies has been a
hallmark of our Hand Service. As an example we will present
our utilization of newly-designed angular stable plates with
Norian bone cement to improve our ability to surgically correct
distal radius malunions in the elderly.
Union with deformity is the most common complication
following a distal radius fracture.(1) This deformity can be
intra-articular, affecting either the radiocarpal or radioulnar
joints; extra-articular characterized by metaphyseal angulation
and loss of length, or it may be a combination of both.(2-6)
Corrective osteotomies have been proven to be an effective
treatment for symptomatic malunion.(1, 7)
A variety of techniques have been used, however there
has remained concern regarding the indications for surgical
intervention in the presence of underlying osteoporosis as well
as the recognized morbidity associated with autogenous iliac
crest bone grafting.(8-10)
Technical advances including the use of precontoured
internal fixation devices with angular stable fixation, as well
as the use of osteointegration biomaterials have offered some
advantages.
The former facilitates osteosynthesis
characterized by higher stability
even in osteopenic bone and
in altered bone architecture as it is
seen in osteoporosis.(11-17) These
implants afford osseous fixation
that allows early motion and rehabilitation.(
18) Also their precontoured
shape maintains desirable
patterns of alignment, congruency
and inclination of the distal radius
after corrective osteotomy because
of their ability to ensure angular and
axial stability.(18-20) These properties
reduce the probabilities of screw
loosening and consequent loss of
reduction.(4, 20)
Following osteotomy and
achievement of proper angulation
and alignment, there will exist a
three-dimensional defect that must
be filled in order to adequately support
the bone fragments.(21-25)
Autogenous bone grafts have been
widely used for this purpose. They have a recognized potential
for donor site morbidity, in particular those involving corticocancellous
variants.(8, 10, 26) Materials such as polymethylmethacrylate
(PMMA) and osteoconductive biomaterials such
as Norian Skeletal Repair System (Norian SRS)? offer structural
support eliminating effects of donor site morbidity.(21-25)
Experience with polymethylmethacrylate (PMMA) has shown
lack of osseous integration.(24, 25) In contrast, prospective
randomized trials demonstrated good clinical and radiological
results with osteoconductive synthetic materials such as Norian
SRS.(21-25)
We believe this operative technique to be safe and predictable.
Additional benefits such as the use in osteoporotic
patients and the elimination of donor site morbidity also support
the practice of this technique.
INDICATION FOR THIS SURGICAL TECHNIQUE
We consider this technique indicated and ideal in the
elderly patient, who is experiencing symptoms and disability
caused by a malunion of a previous distal radius fracture. This
surgery is appropriate to treat these patients, whose bone quality
is not adequate to tolerate any type of implant due to the
presence of osteopenia or osteoporosis.
 MATERIALS AND METHODS MATERIALS AND METHODS
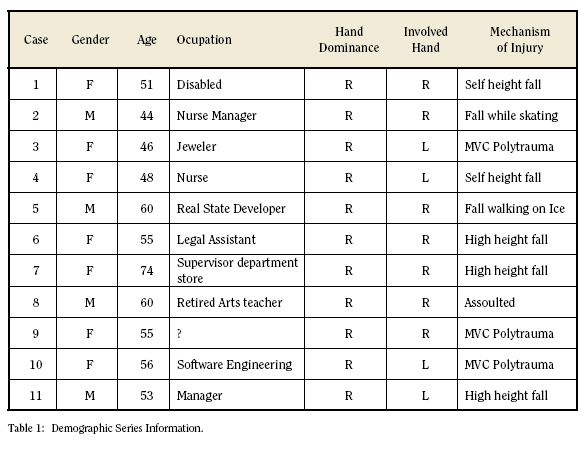
Between 2002 and 2004, 11 patients, 7 female and 4 male
with an average age of 55 years (range: 44 to 74 years), were
treated at Massachusetts General Hospital, Orthopaedic Hand
Surgery Service by a single orthopaedic hand surgeon (J.B.J).
(Table 1)
The patients presented at 8 months post trauma (range:
1 to 14 months) with symptomatic distal radius malunion.
Preoperative clinical and radiological evaluations were done to
assess range of motion, grip and pinch strength and characterize
radiologically the malunion.
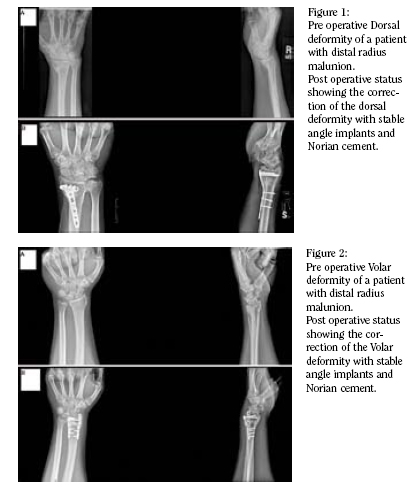
Four patients were classified as “Dorsal” malunion. This
pattern was typified as severe dorsal tilt of the radius in the
lateral plane. (Fig 1) The physical exam of these patients
consistently presented excessive wrist extension and lack or
impairment of wrist flexion. Seven patients were classified as
“Volar” malunion. These were characterized as deformities
with marked volar tilt of the distal radius on the pre-operative
radiography lateral view. (Fig 2) In contrast, these patients had
a lack of wrist extension and greater wrist flexion when compared
to the opposite limb).
The osteotomy was performed trough dorsal approach in
four patients and via volar approach in five; two
had a combined
approach due to excision of previously placed internal
fixation as well as the need for median nerve decompression.
Two corrections included an intraarticular osteotomy.
All cases were performed under regional block anesthesia.
For internal fixation five patients were treated with volar locking
2.4 mm T plates and six with dorsal 2.4 mm. T, L and/or radial
column locking plates. Following the osteotomy and internal
fixation, the created defect was filled with Norian SRS cement?.
X-rays were taken to evaluate quality of reduction and fixation
after the osteotomy. At 10 to 14 days of postoperative immobilization,
all patients started active motion exercises.
Pre and postoperative range of motion and grip strength
were measured by an independent observer. Wrist and forearm
mobility were objectively quantified with a goniometer
(Orthofix, USA). Excellent range of motion was defined as
100% of wrist and forearm motion of the contralateral limb.
Good results as between 75% and 99%; fair between 50% and
74% and bad when achieved motion was less than 50% of the
uninvolved limb. Grip strength was tested also pre and postoperatively,
using a hydraulic hand dynamometer (Baseline?
FEI, Irvington, N.Y. 10533, USA) with the elbow set at the third
station (elbow at ninety degrees of flexion and the wrist and
forearm in neutral). Postoperatively, all patients were measured
according to the Modified Mayo wrist score and the modified
Gartland and Werley score to evaluate outcomes in terms of
pain, ability to return to work, mobility, grip strength, residual
deformities and complications. The DASH questionnaire was
also completed at the postoperative visit.
Ulnar inclination, volar tilt, radial length and ulnar variance
were measured in pre and postoperative radiographs according
to the standard technique for radiographic measurement in the
radius. Percentage improvement and averages were calculated
for each patient.
RESULTS
Corrective osteotomies were performed an average of 8
months after the initial injury (range: 1 – 14 months). There
were no perioperative complications. All osteotomies healed. At
an average follow up of 17 months (range: 6 to 22), 8 patients
of the 11 have completed the evaluation. An average wrist
and forearm motion of 78% of the opposite side was achieved.
Average achieved wrist and forearm motion was 47° degrees of
flexion, 43° of extension, 75° of supination, 86° of pronation,
20° of radial deviation and 35° of ulnar deviation.
The Modified Mayo wrist score scale was used to measure
grip strength. The total of 8 patients were rated as good
strength (strength between 75% and 99%). The grip strength
on average was 88% when compared to the uninvolved hand.
The average grip was 69.8 pounds.
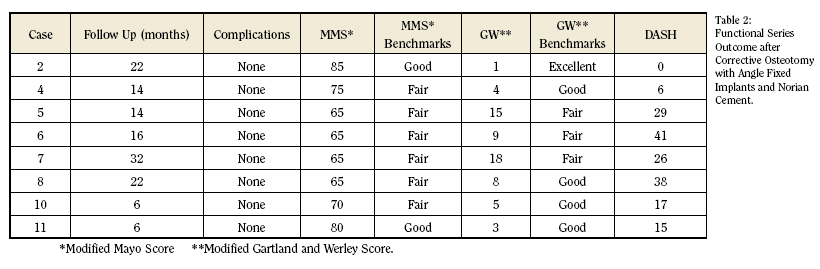
According to the Modified Mayo Wrist Score, two patients
rated as good result (75-89pts) and six as a fair outcome (50-
74pts). There were no patients scoring a bad result (less than
50pts). The average Modified Mayo Wrist Score was 71 points
of a hundred (range: 65-85).(Table 2)
When using the Modified Gartland and Werley Score,
one patient rated as excellent outcome (0-2pts.); four as good
results (3-8pts); and three as a fair result (9-20pts). There
were no poor results (more than 21 pts). The average Gartland
and Werley score was 7.8 points, ranging from 1 to 18 points.
(Table 2)
The average DASH score was 21.5 points, ranging from 0
to 41. (Table 2)
One patient required a Darrach’s procedure at 6 months
to increase motion and management of pain at the distal radio
ulnar joint. Two patients required plate removal due to pain and
limitation in movement. These patients have not completed
their final follow up.
In terms of X ray evaluation the average pre operative volar
tilt was 19.4° in extension in the dorsal deformity group and
25° in flexion in the volar deformity group. Postoperatively,
the average palmar tilt was 12.9° in the former and 12.5° in
the latter group. The average improvement after surgery was
24.6° degrees in patients with dorsal deformity and 14.1° in
those with volar deformity. Pre operative ulnar variance was on
average 4.1 mm, after surgery it corrected to 2.54 mm (50%).
Ulnar inclination averaged 14.5° preoperatively, after treatment
it averaged 22° presenting an improvement of 7.5°. Lastly,
with the exception of one patient, restoration after surgery
achieved acceptable clinical outcomes and radiologic parameters.
Assessment for posttraumatic arthritis was negative in
every case at the time of follow up.
DISCUSSION
A corrective osteotomy in the older patient is more difficult
because of the associated osteopenia as well as the limited
autogenous bone graft to be obtained from the iliac crest.
Several technological advances have made this procedure more
predictable. The first is the development of low profile implants
with angular stable screw fixation. This osteosynthesis system
device has shown good results in maxillofacial and spine
surgery, where stability is required without bicortical screw
purchase.(13, 16, 17)
The locking compression system offers a similar mechanism
of action with the mechanical advantage of multiple
points of screw fixation when compared to fixed angle devices.
It is a point of crucial importance in fractures with long working
lengths, short periarticular fragments and the absence of
osseous support on the contralateral side where the plate is
placed.(13) The angle fixed constructs do not affect the blood
supply to the bone and do not require good bone quality to proportionate
stability. In this system, threads on the screw heads
lock into the corresponding threads on the screw hole of the
plate, eliminating therefore toggling. Forces are transmitted
then from the bone to the plate across the threaded connection
converting compression unnecessary to get stability. This
lack of compression preserves the blood supply to the bone
improving conditions for healing. Disadvantages of this system
include no tactile feedback to the surgeon while tightening the
screws. Previous reduction is needed before application of the
device, once the locked screw is placed below or above of the
fracture site no further reduction is possible unless the construct
is totally removed.(27-30) Clinical trials have verified the
efficacy of fixed angled plates for the treatment of distal radius
fractures. (27-30) Functional outcomes are promising and the
rate of complications low, making this implant desirable also
for the stabilization of osteotomies for the treatment of distal
radius malunion.
The second technical advance is the use of cement and
biomaterials that can support and put together fragments of
bone, and that can fill defects after severe comminution or
osteotomies. The role of this material is particularly important
in osteoporotic bone that cannot tolerate adequately constructs
and that needs support while consolidation process takes place.
Norian SRS Cement offers biocompatibility and osteointegration;
high compressive strength, even higher than cancellous
bone; fast-setting that cures in vivo at physiological pH and
temperature avoiding local damage tissue characteristic of
PMMC use; and lastly injectable consistency that allows percutaneous
as well as open-technique application.(24)
Additionally, advantages in imaging under fluoroscopy and
X rays have been proved.(9, 31)
Two prospective randomized studies (Sanchez-Sotelo et
al and Cassidy et al) evaluating the use of Norian showed good
results.(21, 24) Clinical outcomes were significantly better
than the standard care; however, none of them defined what
type of fractures gets benefit from this particular approach with
cement and percutaneous fixation. Recent research has demonstrated
comparable results between percutaneous fixation
and open reduction and internal fixation for extra articular and
non-complex intraarticular fractures(30), therefore, the role of
Norian? cement in distal radius fractures in previous studies
must be related with bone quality, in other words, osteoporosis
and osteopenia.
According to the mechanism of action and previous
description of these two surgical advances, we consider them
extremely useful for the treatment of malunions in osteopenic
patients that suffered a distal radius fracture concluding in
malunion or mal-alignment. We find this technique useful and
safe to treat malunion.
CONCLUSION
This series reports the results of treatment of distal radius
malunion with osteotomy plus internal fixation with locking
compression plates and Norian SRS?. Our purpose is to present
this technique as an alternative in these complex cases where
we have to face the elderly patient with osteoporotic bone.
Santiago A. Lozano-Calderón, MD is a Research Fellow, Orthopaedic Surgery Service, Harvard Medical School, Massachusetts General Hospital, Boston, MA.
Jesse B. Jupiter, MD is Chief Orthopaedic Hand Surgery Service, Harvard Medical School, Massachusetts General Hospital, Boston, MA.
Address correspondence to:
Jesse Jupiter, M.D.
Massachusetts General Hospital
55 Fruit St., YAW2
Boston, MA 02114
References:
- Fernandez DL, Ring D, Jupiter JB. Surgical management of delayed union and nonunion of distal radius fractures. J Hand Surg [Am]. 2001 Mar;26(2):201-9.
- Shea K, Fernandez DL, Jupiter JB, Martin C, Jr. Corrective osteotomy for malunited, volarly displaced fractures of the distal end of the radius. J Bone Joint Surg Am. 1997 Dec;79(12):1816-26.
- Martini AK. Secondary arthrosis of the wrist joint in malposition of healed and un-corrected fracture of the distal radius. Aktuelle Traumatol. 1986 Aug;16(4):143-8.
- Miyake T, Hashizume H, Inoue H, Shi Q, Nagayama N. Malunited Colles’ fracture. Analysis of stress distribution. J Hand Surg [Br]. 1994 Dec;19(6):737-42.
- Pogue DJ, Viegas SF, Patterson RM, Peterson PD, Jenkins DK, Sweo TD, et al. Effects of distal radius fracture malunion on wrist joint mechanics. J Hand Surg [Am]. 1990 Sep;15(5):721-7.
- Villar RN, Marsh D, Rushton N, Greatorex RA. Three years after Colles’ fracture. A prospective review. J Bone Joint Surg Br. 1987 Aug;69(4):635-8.
- Jupiter JB, Fernandez DL. Complications Following Distal Radial Fractures. Journal of Bone and Joint Surgery. 2001 August;83-A(8):1244-65.
- Hill NM, Horne JG, Devane PA. Donor site morbidity in the iliac crest bone graft. Aust N Z J Surg. 1999 Oct;69(10):726-8.
- Kopylov P, Jonsson K, Thorngren KG, Aspenberg P. Injectable calcium phosphate in the treatment of distal radial fractures. J Hand Surg [Br]. 1996 Dec;21(6):768-71.
- Silber JS, Anderson DG, Daffner SD, Brislin BT, Leland JM, Hilibrand AS, et al. Donor site morbidity after anterior iliac crest bone harvest for single-level anterior cervical discectomy and fusion. Spine. 2003 Jan 15;28(2):134-9.
- Ring D, Jupiter JB, Brennwald J, Buchler U, Hastings H, 2nd. Prospective multicenter trial of a plate for dorsal fixation of distal radius fractures. J Hand Surg [Am]. 1997 Sep;22(5):777-84.
- Gesensway D, Putnam MD, Mente PL, Lewis JL. Design and biomechanics of a plate for the distal radius. J Hand Surg [Am]. 1995 Nov;20(6):1021-7.
- Haidukewych GJ. Innovations in locking plate technology. J Am Acad Orthop Surg. 2004 Jul-Aug;12(4):205-12.
- Frigg R, Appenzeller A, Christensen R, Frenk A, Gilbert S, Schavan R. The development of the distal femur Less Invasive Stabilization System (LISS). Injury. 2001 Dec;32 Suppl 3:SC24-31.
- Koval KJ, Hoehl JJ, Kummer FJ, Simon JA. Distal femoral fixation: a biomechanical comparison of the standard condylar buttress plate, a locked buttress plate, and the 95-degree blade plate. J Orthop Trauma. 1997 Oct;11(7):521-4.
- Richter M, Wilke HJ, Kluger P, Claes L, Puhl W. Biomechanical evaluation of a newly developed monocortical expansion screw for use in anterior internal fixation of the cervical spine. In vitro comparison with two established internal fixation systems. Spine. 1999 Feb 1;24(3):207-12.
- Herford AS, Edward EI. Use of a Locking Reconstrucion Bone Plate/Screw System for Mandibular Surgery. J Oral Maxillofac Surg. 1998;56:1261-5.
- Jupiter JB. Complex Articular Fractures of the Distal Radius: Classification and Management. J Am Acad Orthop Surg. 1997 May;5(3):119-29.
- Simic PM, Weiland AJ. Fractures of the distal aspect of the radius: changes in treatment over the past two decades. Instr Course Lect. 2003;52:185-95.
- Trumble TE, Randall C. Intra-articular fractures of the Distal Aspect of the Radius. The Journal of Bone and Joint Surgery. 1998 April 1998;80-A(4):582-600.
- Sanchez-Sotelo J, Munuera L, Madero R. Treatment of fractures of the distal radius with a remodellable bone cement: a prospective, randomised study using Norian SRS. J Bone Joint Surg Br. 2000 Aug;82(6):856-63.
- Constantz BR, Ison IC, Fulmer MT, Poser RD, Smith ST, VanWagoner M, et al. Skeletal repair by in situ formation of the mineral phase of bone. Science. 1995 Mar 24;267(5205):1796-9.
- Larsson S, Bauer TW. Use of injectable calcium phosphate cement for fracture fixation: a review. Clin Orthop. 2002 Feb(395):23-32.
- Cassidy C, Jupiter JB, Cohen M, Delli-Santi M, Fennell C, Leinberry C, et al. Norian SRS cement compared with conventional fixation in distal radial fractures. A randomized study. J Bone Joint Surg Am. 2003 Nov;85-A(11):2127-37.
- Cohen MS, Whitman K. Calcium phosphate bone cement--the Norian skeletal repair system in orthopedic surgery. Aorn J. 1997 May;65(5):958-62.
- Ahlmann E, Patzakis M, Roidis N, Shepherd L, Holtom P. Comparison of anterior and posterior iliac crest bone grafts in terms of harvest-site morbidity and functional outcomes. J Bone Joint Surg Am. 2002 May;84-A(5):716-20.
- Orbay JL. Volar plate fixation of distal radius fractures. Hand Clin. 2005 Aug;21(3):347-54.
- Orbay JL. The treatment of unstable distal radius fractures with volar fixation. Hand Surg. 2000 Dec;5(2):103-12.
- Orbay JL, Fernandez DL. Volar fixed-angle plate fixation for unstable distal radius fractures in the elderly patient. J Hand Surg [Am]. 2004 Jan;29(1):96-102.
- Kreder HJ, Hanel DP, McKee M, Jupiter J, McGillivary G, Swiontkowski MF. Consistency of AO fracture classification for the distal radius. J Bone Joint Surg Br. 1996 Sep;78(5):726-31.
- Jupiter JB, Winters S, Sigman S, Lowe C, Pappas C, Ladd AL, et al. Repair of five distal radius fractures with an investigational cancellous bone cement: a preliminary report. J Orthop Trauma. 1997 Feb-Mar;11(2):110-6.
|