Functional Outcomes of Scapholunate Diastases Associated with Distal Radius Fractures
Jonathan Lans, MD, Alejandro Lasa, MD, Neal C. Chen, MD, Jesse B. Jupiter, MD
The authors report no conflict of interest related to this work.
©2018 by The Orthopaedic Journal at Harvard Medical School
BACKGROUND The scapholunate interosseous ligament (SLIL) plays an important role in the scapholunate joint. The SLIL is often the first intrinsic carpal ligament to be injured in wrist trauma and injuries have been noted in up to 64% of distal radius fractures. However, it remains unclear which patients develop symptoms. The natural history of SLIL, when associated with a distal radius fracture, is unclear and primary treatment of these injuries remains in debate. Our hypothesis was that scapholunate diastases associated with distal radius fractures are rarely clinically relevant. To evaluate this the incidence of unilateral scapholunate diastases were assessed along with the functional outcomes.
METHODS We evaluated 391 patients with a distal radius fracture treated operatively from 2007 to 2015. The scapholunate interval (SLI) and the scapholunate angle (SLA) were measured using CT scans. A scapholunate diastasis (SLD) was defined as an SLI of ≥3mm. We identified 14 (3.6%) patients with a SLD of the injured wrist who all then underwent a CT scan of the contralateral wrist, to assess for pre-existing bilateral SLD. Only 6 patients had a unilateral SLD. We performed a bivariate analysis to compare if the SLI or SLA increased between initial and final follow up, with a mean radiographic follow up of 91 months. To evaluate the functional outcomes at mean follow up of 136±90 weeks we used the Quick Disabilities of the Arm, Shoulder and Hand (qDASH) Score, higher scores indicating increasing disability.
RESULTS There were 8 patients (57%) with bilateral SLD diagnosed in CT scan. The 6 patients with a unilateral SLD did not show a significant increase in SLI or SLA at final follow up. Five patients had a qDASH score of 0 and one patient showed a qDASH score of 18.2. The patient with a poor score had bilateral preexisting osteoarthritis of the wrist. No patient had surgery to repair SLIL injury.
CONCLUSION In patients with a SLI of ≥3mm associated with a distal radius fracture, more than half had bilateral SLD by radiographic criteria. It is therefore worthwhile to image the contralateral wrist before diagnosing a true SLD. Most patients with unilateral SLD in this setting do not appear to require surgical management of the SLD at initial presentation because they have good functional outcomes with non-operative care after a follow up of 2 years.
LEVEL OF EVIDENCE
KEYWORDSOscapholunate ligament, scapholunate dissociation, distal radius
Scapholunate interosseous ligament (SLIL) injury occurs in combination with distal radius fractures in up to 64% of cases.1-8 It is an important link between the scaphoid and the lunate.9 SLIL injury can lead to scapholunate dissociation (SLD), which occasionally leads to a scapholunate advanced collapse (SLAC) wrist arthritis pattern.6,10-14 It is unclear whether SLIL repair or reconstruction can prevent progression to arthrosis.15
In the acute posttraumatic radiographs of distal radius fractures a scapholunate diastasis (>3mm) is often seen.8,16,17 However, these may not always be clinically relevant. It is possible that ligamentous healing takes place during immobilization of the distal radius fracture.4,18,19 Alternatively, some studies report simultaneous open distal radius fixation and direct SLIL reconstruction in the presence of an acute SLD.20-24
Based on clinical experience, we hypothesized that acute scapholunate diastasis in the setting of distal radius fractures is infrequent and rarely impairs function. Therefore, the aim of this study was to determine the incidence of unilateral SLD’s associated with distal radius fractures and to evaluate the functional outcomes of these patients.
Study Population
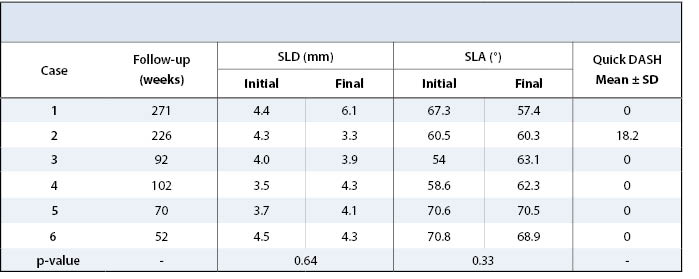
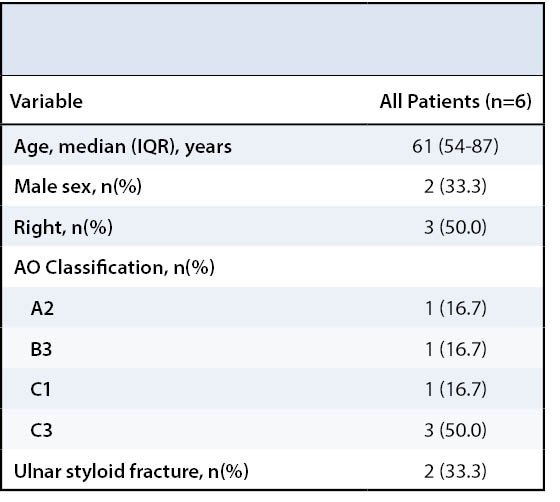
After institutional review board approval, we retrospectively evaluated all distal radius fractures (n=391) from 2007 to 2015 that were treated in the British Hospital of Montevideo, Uruguay. These were identified through an ongoing procedural database maintained by the traumatology department that collects patient and treatment data prospectively. Patients with an unacceptably reduced fracture position were operatively treated using a volar approach with volar variable angle plate fixation. The scapholunate joint was not surgically treated in any patient. All patients underwent a postoperative computed tomography (CT) scan. We defined a SLD as an SLI of ≥3mm, based on the correlation between Geissler grade 3 and 4 tears and a radiographic SLI of ≥3mm.25 We excluded one patient with bilateral distal radius fractures. We only included patients (n=14, 3.6%) with a scapholunate interval (SLI) of ≥3mm in the injured wrist in analysis as these all underwent a CT scan of the contralateral wrist. Of these patients, 8 (57%) also had a contralateral SLI ≥3mm suggesting anatomic variance rather than a true scapholunate injury in the operative wrist. Of the 6 patients with unilateral SLD, we report on 2 males and 4 females, with a median age of 61 (range: 54-87) years with an average radiographic follow-up of 109±91 weeks (range: 26-245) and average functional follow-up of 136±90 weeks (range: 52-271) (Table 1). There were 3 type C3 fractures, 1 type C1 fracture, 1 type B2 fracture and 1 type A2 fracture. There was an associated ulna fracture in 2 patients.
Evaluation
CT scan (SOMATOM Emotion 16, Siemens Healthcare, Malvern, Pennsylvania, USA) images of the wrist were obtained post-operatively and at final radiographic follow-up. Measurements were performed using OsiriX Viewer (Pixmeo SARL, Bernex, Switzerland). The scapholunate interval (SLI) was measured positioning the CT beam parallel to the SLI in the axial plane (Figure 1). The thickness of the CT slices were digitally increased to a width between 7-14mm to evaluate the SLI and the scapholunate angle (SLA), this allows for visualization of the lunate and scaphoid in one image. We measured the SLI from the midpoint of the lunate to the midpoint of the scaphoid in the coronal plane. Scapholunate diastasis was defined as a SLI ≥3mm. The SLA was evaluated in the sagittal plane by calculating the angle between the scaphoid axis and the lunate axis. (Figure 2). The functional outcomes were evaluated using the Quick Disabilities of the Arm, Shoulder and Hand (qDASH).
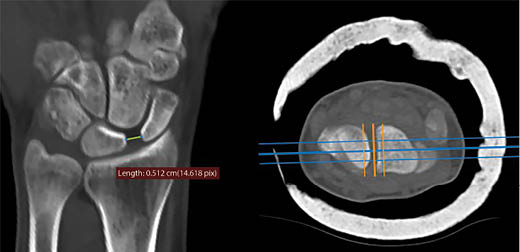
Using the OsiriX Viewer, a coronal slice is created at the level where the antero-posterior CT beam (middle orange line) is parallel to the scapholunate interval.

Statistical Analysis
Continuous data were stated as mean ± standard deviations and categorical data as frequencies and percentages. We used a paired student’s t-test to compare the differences between SLI distances and SLA in the immediate post-operative CT scan compared to the CT scan at final follow-up.
The average post-operative SLI was 4.1±0.4mm and the average SLI at final follow-up was 4.3±0.9mm (p=0.51) (Table 2). The average post-operative SLA was 63.8±5.0° and at final follow-up this was 63.6±6.9° (p=0.97, Table 2). Five patients had a Quick DASH score of 0 and one patient had a score of 18.2, but this patient had severe preexisting degenerative osteoarthritis of the injured wrist. No patient required additional surgery of the SLIL.
In this study, we evaluated the scapholunate interval (SLI) in 391 patients with a distal radius fracture who underwent volar plate fixation. Using a computer tomography of the wrist we measured the SLI, defining a scapholunate diastasis when the SLI was ≥3mm. Of all the distal radius fractures, there were 14 patients with a SLD, of which 8 showed a SLI of >3mm in the contralateral wrist. We identified 6 patients with true unilateral SLD’s in the injured wrist, possibly due to a SLIL tear. None of the patients with unilateral SLD had operative treatment of their scapholunate joint at time of distal radius fixation. After an average follow-up of more than two years, 5 out of 6 patients reported an excellent qDASH score. The patient with increased disability on the qDASH had preexisting bilateral degenerative osteoarthritis of both wrists, which we suspect may be a contributing factor in experiencing more pain in the injured wrist. The value of this study is that this is the first study using bilateral CT scans to compare the SLI after a distal radius fracture.
Distal radius fractures are often accompanied with ligamentous injury, most frequently triangular fibrocartilage complex injuries, but second most frequently SLIL injuries.1,3,5,22,25-31 The scapholunate interosseous ligament is the most important stabilizer of the scapholunate joint.9,32 Mudgal and Jones emphasized for surgeons to be aware of a SLIL injury in the presence of a fracture line between the scaphoid- and lunate fossa.23 Furthermore, Mudgal et al. advised treatment of scapholunate diastases when present as part of four-part distal radius fractures.24 Others have suggested scapholunate fixation for Geissler grade 3 and grade 4 SLIL tears.20-22 It is however, still unknown which patients with SLIL injury develop scapholunate advanced collapse (SLAC) and which patients develop symptoms.6,10 In a study by Fassler et al. 73% of the patients with radiographic evidence for a SLAC did not report pain.11
The gold standard to diagnose scapholunate tears is arthroscopy.33 Using this modality, scapholunate tears associated with distal radius fractures occur in 7-64% patients.1,3,5,6,20,22,25,26,29,30,34,37 The incidence of concomitant SLIL is lower in extra-articular fractures (7-33%).2-4,38 Arthroscopically assisted distal radius fracture treatment allows confirmation of SLIL tears, but many of these lesions seem to be clinically irrelevant.1,6 Repeated arthroscopies to evaluate ligament healing would be ideal but are an unacceptable burden for patients and have therefore not been performed. In conventional anteroposterior radiographs, SLD is often defined as a SLI of equal to or more than 2- or 3mm. Incidences reported using ≥2mm range from 26-52%, whereas studies using ≥3mm report incidences of 5-8%.4,8,10,16,17,38,39 After distal radius fracture reduction many SLD’s may resolve, possibly due to ligamentotaxis.4
Geissler et al. showed that Geissler grade 3 or 4 lesions had a radiographic SLI of ≥3mm.25 Therefore we chose ≥3mm to define a SLD as we considered this clinically relevant. Using the CT scan, we found an incidence of SLD in 1.5% of the patients, which is lowest reported incidence to date. Furthermore, we found that 57% of the SLD’s were bilateral which is similar to prior literature where this has been reported to be present in 38-52%.10,40 We believe that if a radiographic cut-off for SLD of ≥2mm is used, many clinically irrelevant increased scapholunate intervals will be diagnosed.
Outcomes regarding SLD’s associated with distal radius fractures are contradictory. Several reports with a follow-up of one year have shown no differences between patients with or without SLD accompanying a distal radius fracture.1,26,38 However, Tang et al. showed significantly increased SLI’s after one year follow-up in 20 patients treated with cast immobilization and that 8 patients underwent SLIL treatment within one year.17 They suggested that a SLI of ≥3mm along with the presence of additional signs of carpal instability such as the cortical ring sign, a scapholunate angle >70° and foreshortening of the scaphoid are indicative for severe injury.
Longer term studies seem to favor conservative treatment of SLD’s associated with distal radius fractures. Mrkonjic et al. evaluated arthroscopically diagnosed scapholunate tears after 13-15 years of follow up after conservative treatment.6 They concluded there was no difference in objective or subjective outcomes in patients with Geissler grade 3 tears compared to grade 1-, grade 2- or no tears. These findings were confirmed by Finsen et al. that defined SLD as a SLI ≥2mm in conventional radiographs of extra-articular distal radius fractures and evaluated the outcomes of 12 patients after a mean follow-up of six years.39 They concluded that the outcomes with or without SLD were similar. Added to that, scapholunate fixation along with distal radius fixation does not seem to improve functional outcomes at four years follow up.41
However, we need to interpret these results in respect to their strengths and limitations. First, we did not compare the outcomes of patients with a SLD to those without a SLD. Second, CT scans are not standard clinical practice in all settings and our results are not applicable for conventional radiographs. The advantage of using CT scans is that they allow the evaluator to precisely position the radiographic beam parallel to the scapholunate joint avoiding measurement errors due to angulated views of the wrist. Suzuki et al. reported a sensitivity of 75% and specificity of 90% using CT scans to measure the SLI.42 The value of this study is that this is the first study using bilateral CT scans to compare the SLI in both wrists after a distal radius fracture. However, interrater reliability was not assessed as only one observer measured radiographs. Third, this study had a small sample size making it underpowered. Lastly, the radiographic follow up ranged from 26 to 245 weeks, where two patients had a follow up of less than one year. Dynamic instability can develop after one year but the development of SLAC can take three to 15 years.43
In conclusion, we have highlighted the importance of bilateral wrist imaging when concerned for SLD as 57% of the wrists showed bilateral scapholunate intervals of ≥3mm. Furthermore, we showed that patients with distal radius fractures that underwent surgical volar plate fixation and no treatment of the scapholunate interosseous ligament had excellent patient reported outcomes. These results along with the presented literature suggests that initial treatment of a SLI of ≥3mm does not require treatment when accompanying a distal radius fracture. Further studies with truly long term functional outcomes are needed to increase our understanding of the consequences of scapholunate interosseous ligament injuries.