Assessment of Current Narcotic Prescriptions in Orthopaedics at Boston Children’s Hospital
Susan T. Mahan, MD, MPH, Lanna Feldman, MS, Clarissa Cheng, Rachel L. DiFazio, PhD, RN, PPCNP-BC, FAAN
The authors report no conflict of interest related to this work.
©2017 by The Orthopaedic Journal at Harvard Medical School
OBJECTIVE Due to concern with increasing opioid addiction in the community, legislative changes in Massachusetts opioid prescription laws, and the potential of our contribution to society’s excess opioid load, we assessed the current status of opioid prescriptions in our department.
METHODS Current residents, fellows and mid-level providers were asked to complete a questionnaire on opioid prescribing practices. Additionally, our hospital’s data system was queried to identify all post-operative patients in a 5-month period in 2015 and 2016 to assess prescriptions and refill prescriptions; these were analyzed both as individual numbers of pills as well as converted to patient doses. Comparison from 2015 to 2016 for all surgeries, as well as more detailed analysis specifically for anterior cruciate ligament (ACL) reconstruction, peri-acetabular osteotomy (PAO), adolescent idiopathic scoliosis (AIS) and supracondylar humerus fracture (SCH).
RESULTS 29/38 eligible healthcare providers participated in the online survey (76%). The most common post-operative prescription reported was for 25-50 doses in 52% of responders. The total number of tablets prescribed by our department decreased by 19% in 2016 (93,181) when compared to 2015 (114,755). When compared by procedure, all doses of oxycodone decreased in 2016 when compared to 2015 in AIS (2015 mean 70.6, standard deviation 32.5; 2016 mean 46.9, SD 15.9; P<0.001), SCH (2015 mean 33.5, SD 16.3; 2016 mean 22, SD 11; P<0.0001), PAO (2015 mean 59.1, SD 28.2; 2016 mean 46.7, SD 16.9; P=0.0190) and ACL (2015 mean 52, SD 19; 2016 mean 43.3, SD 10.2; p<0.001). Refill prescriptions increased notably in spine and tumor surgery.
CONCLUSION Post-operative narcotic prescriptions decreased in our department from 2015 to 2016 after the Massachusetts legislation. Spine and tumor surgery saw a notable increase in refills. Further work including actual narcotic usage should be done to better understand post-operative needs and further streamline these prescriptions.
LEVEL OF EVIDENCE Level IV, Cross sectional survey
KEYWORDS Opioid, narcotic prescriptions, Massachusetts legislation
In the 1990’s, pain was suggested to be the 5th vital sign. This resulted in an increased awareness of the need to assess and treat patients’ pain.1 In the late 1990’s, there was a dramatic increase in the number of prescriptions written for opioids in the United States.2 This was followed, shortly after the turn of the century, by a sharp increase in unintentional opioid overdoses and poisonings.3 This change in prescribing practice has occurred throughout the country, as well as locally in Massachusetts.4 In an attempt to address this epidemic, Massachusetts Governor Charlie Baker signed legislation to limit opioid prescriptions on March 14th, 2016.5,6 This bill includes:5,7
- Limiting opioid prescriptions to seven days except in the setting of chronic pain
- Initiating a state prescription monitoring program that went into effect in October 2016
- Allowing patients to have a “partial fill” of their prescription
In the Orthopaedic Department at Boston Children’s Hospital, narcotics are routinely prescribed to adolescents and young adults who have undergone orthopaedic surgery for trauma, injury, deformity or tumor. Adolescents are at risk for becoming addicted to opioids and increased opioid abuse in adolescents is associated with an increased rate of narcotic prescriptions.8,9 Additionally, opioid deaths, particularly in Massachusetts, are highest in the 25-34 year old age group.10 Adolescents are known to utilize “leftover” prescription opioids on a nonmedical or recreational basis.11 Therefore, supplying this age group with a large amount of opioid narcotics, even after appropriate orthopaedic surgery, is concerning.
In our department, the majority of opioid narcotics are prescribed in the post-operative period, typically by the first assistant of the case; usually a resident, fellow or physician assistant (PA). If a patient runs out of narcotics while still having post-operative pain, refills can be provided through our nursing triage line. By law, a paper copy of the prescription must be provided; this can be picked up in person, placed in the standard U.S. Mail, or sent by an overnight courier services. Mailing a prescription for a refill to a family using an overnight courier service can be costly; $18-$48 per prescription. Nursing estimates have noted that our department has spent an average of $1200 per week to mail prescriptions to families; the department has since changed its policies regarding refills.
The purpose of this quality improvement project was to assess the current status of narcotic prescribing in the Department of Orthopaedics at Boston Children’s Hospital in order to have a basis of comparison for future initiatives. With the implementation of the new Massachusetts state opioid law, comparisons from before and after implementation of the law could be made in prescribing practices. We sought to:
- Assess current narcotic prescribing patterns and influences with an anonymous query of the residents, fellows, nurse practitioners (NP), and physician assistants (PA)
- Assess the total number of post-operative prescriptions written and the total number of doses prescribed per patient; comparing 2015 (prior to the new law) and 2016 (after the new law went into effect) using a Boston Children’s Hospital database.
This was a quality improvement project. Two different phases were involved in this project and the methods for each phase will be described separately.
Survey for residents, fellows and mid-level providers
A Research Electronic Data Capture (REDCap) questionnaire was designed to assess prescribing patterns and factors influencing prescribing. The current rotating residents, fellows (pediatric, hip, and operative sports), NPs and PAs in the Orthopaedic and Sports Medicine Department at Boston Children’s Hospital were asked to complete the online survey. Answers were anonymous, but it could be determined which participants had completed the survey in order to re-cue non-responders to fill out the survey.
Questions on the online survey included current level of training, estimated weekly frequency of operative cases and post-operative prescribing, estimated weekly frequency of writing narcotic prescription refills, estimated average number of doses prescribed, type of cases typically covered (e.g. spine, peri-acetabular osteotomy (PAO), anterior cruciate ligament (ACL) reconstruction, and supracondylar humerus (SCH) fracture reduction and fixation). Participants were also asked about what factors influence the number of narcotic pills/liquid they prescribe, whether or not they tell families what to do with excess pills/liquid, whether or not they discuss narcotic weaning with patients/families, if they council patients/families on side effects, and if the new Massachusetts law limiting first time prescriptions to only 7 days influenced their prescribing practices.
Data analysis was done utilizing descriptive statistics through the REDCap program.
Global assessment of orthopaedic department post-operative prescriptions
Childrens360 enterprise data warehouse system was used to identify all post-operative orthopaedic prescriptions written from April through August 2015 and April through August 2016. This data range was chosen because the new Massachusetts opioid law went into effect in March 2016 and we wanted to assess for any change that occurred after the new law went into effect. The total number of prescription refills was also collected, but was analyzed separately. Refills were determined by noting that the date of the prescription was after the date of discharge. The vast majority of the prescription refills were either for a narcotic (e.g. oxycodone or hydrocodone) or a benzodiazepine. Oxycodone is prescribed in the post-operative setting except in infrequent situations. For the purposes of this analysis, a dose of oxycodone was considered equivalent to a dose of hydrocodone.Non-addicting prescriptions, such as acetaminophen or ibuprofen, were removed from the analysis. If multiple prescriptions were entered for a patient prior to discharge, only the prescriptions entered just prior to discharge were chosen. Demographic data including age, gender and race were also obtained.
As prescriptions in the pediatric population are often given as a liquid solution, these were converted to doses based on patient weight and individual prescription specifics. Number of tablets were counted individually and converted to dosage based on the individual prescription (for example, if the prescribed medication was provided in 5 milligram (mg) tablets, with instruction to take 2 tablets at a time, then the individual tablet count is 2, while the dose is 10 mg). This data was compared for all procedures from 2015 to 2016, as well as across selected procedures: ACL reconstruction, PAO, spinal fusion for adolescent idiopathic scoliosis (AIS) and surgical repair of SCH fractures.
A separate analysis on the prescription refills was done to assess pattern changes from 2015 to 2016. Procedural categories were established, such that “spine” category encompassed all post-operative spine cases (including neuromuscular, idiopathic, and other), “open hip” category encompassed all hip cases where an open procedure was performed (e.g. pelvic and/or femoral osteotomies), “fracture” category encompassed all operative fracture care. These procedural categories do not match the more stringent categories above for ACL, PAO, SCH and AIS.
Data was initially compared in Excel (Microsoft Corporation), with additional data analysis in GraphPad Prism 6.0 for Mac OS (LaJolla, CA, USA). Statistical significance was set a priori at p<0.05, two tailed. Descriptive statistics were determined using Excel and comparisons of data were done using GraphPad Prism and Student’s t-test, with variance assessed and determined to be reasonably similar.
Query for residents, fellows and mid-level providers
Out of a total of 38 eligible participants twenty-nine (76%) people completed the online survey. Of the respondents, 24% were orthopaedic fellows (7/29), 17% were orthopaedic residents (5/29), 28% were orthopaedic physician assistants (8/29) and 31% were orthopaedic nurse practitioners (9/29). Forty-one percent of respondents (12/29) reported that they typically do not scrub in the operating room (OR), while 14% typically cover 1-3 surgical cases per week (4/29), 31% typically cover 3-8 surgical cases per week (9/29) and 14% typically cover more than 8 surgical cases a week (4/29). The respondents reported writing post-operative narcotic prescriptions (not including refills): never in 21% (6/29), 1-3 prescriptions per week in 17% (5/29), 3-8 prescriptions per week in 38% (11/29) and more than 8 prescriptions per week in 24% (7/29). They reported writing narcotic refills: never in 41% (12/29), 1-3 prescriptions per week in 55% (16/29), and 3-8 prescriptions per week in 3% (1/29). The most common prescription reported being written is for 25-50 doses per prescription in 52% (15/29), followed by 10-25 doses per prescription in 31% (9/29), less than 10 doses per prescription in 10% (3/29) and more than 50 doses per prescription in 7% (2/29).
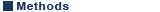
Respondents were asked what factors influence the number of narcotic pills they prescribe, and they could check all factors that apply (Figure 1). When ranking these choices, the most popular factor (76% ranked as either their first or second factor) was the desire for patients’ pain to be controlled in the post-operative period. The second choice of the rankings of factors (52% ranked as either their first or second factor) was prescribing what they think the patient will require.
Ranking of top five chosen options for when survey respondents were asked what factors influence the number of narcotic pills they prescribe. They could check all factors that apply.
When asked if they tell patients/families what to do with excess narcotic pills, 43% (12/28) reported sometimes, 46% (13/28) reported no, and 11% (3/28) reported always; one person did not respond. When asked if they discuss narcotic weaning with patients/families, 57% (16/28) reported always, 39% (11/28) reported sometimes, and 4% (1/28) reported no; one person did not respond. When asked if they ever council patients/families on side effects, 89% (25/28) reported yes while 11% (3/28) reported no; one person did not respond. When asked if the new Massachusetts law limiting first time prescriptions to only 7 days has influenced their prescribing practices, 71% (20/28) reported yes while only 29% (8/28) reported no; one person did not respond.
Global assessment of orthopaedic department post-operative prescriptions
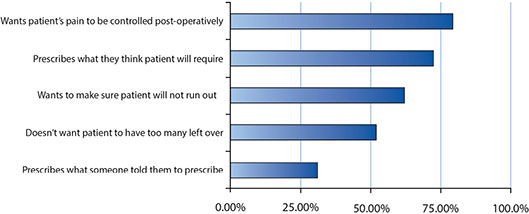
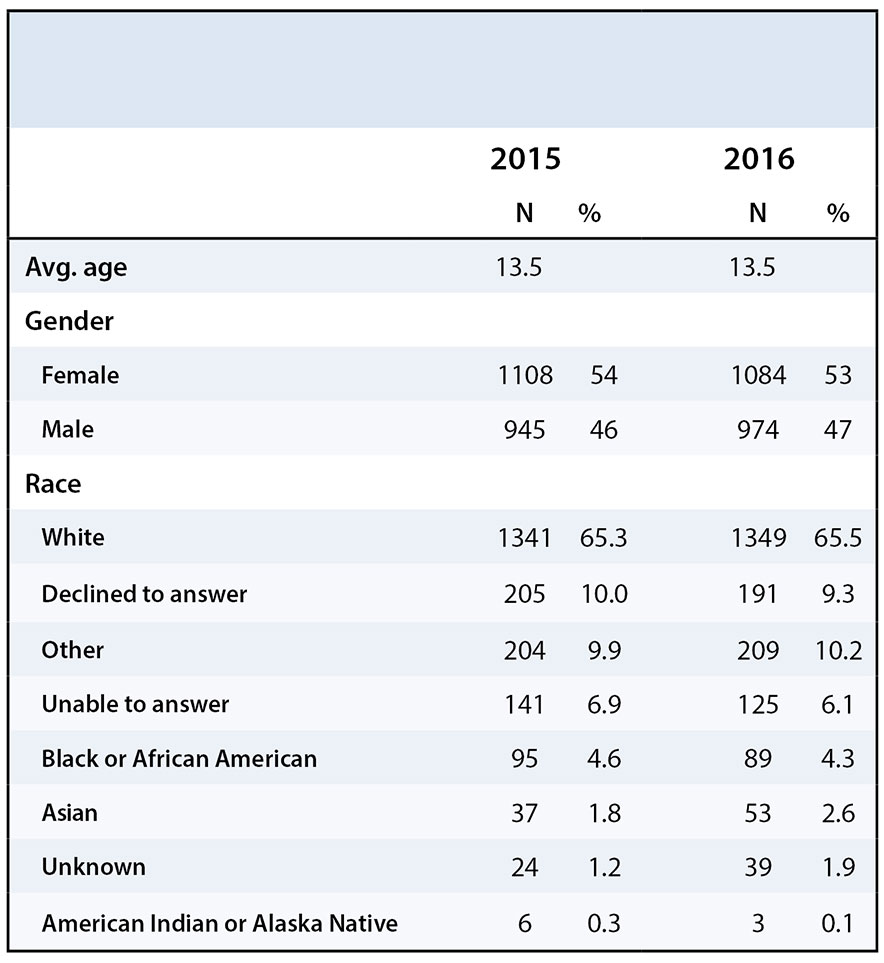
The number of prescriptions, surgeries, and patients undergoing surgeries remained consistent from 2015-2016 (Table 1). From 2015 to 2016 basic demographics, including age, gender and race were also consistent (Table 2). However, the total number of tablets prescribed by the Department of Orthopaedics decreased from 114,755 in 2015 to 93,181 in 2016. This represents a 19% decrease in the total number of tablets prescribed to our patients. The number of diazepam tablets decreased from 30,209 to 29,306, and the number of oxycodone tablets fell from 79,546 to 63,875.
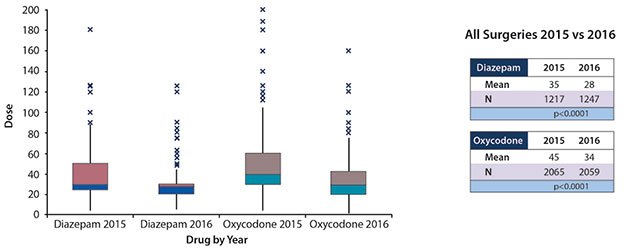
In the analysis comparing all surgeries between 2015 and 2016, the average prescribed dose for both diazepam and oxycodone decreased significantly (Figure 2). Diazepam decreased from an average of 35 doses per patient to 29 doses (p<0.0001; 95% confidence interval -8.1 to -5.5), and oxycodone decreased from an average of 45 doses per patient to 34 doses (p<0.0001; 95% CI -12.5 to -9.9).
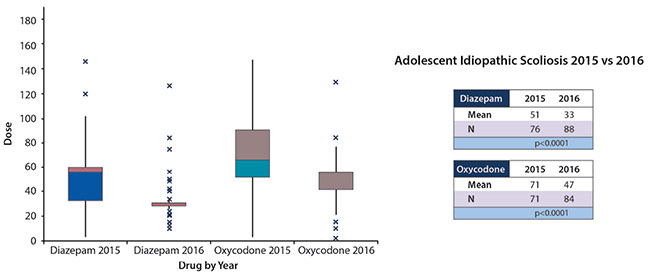
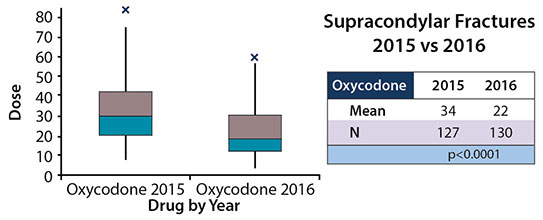
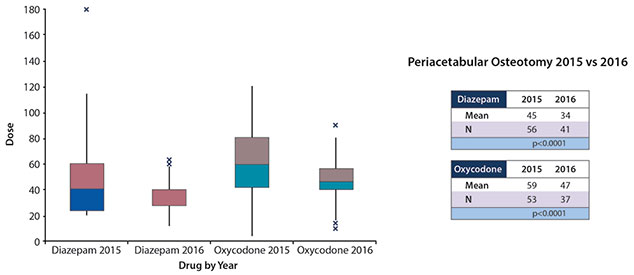
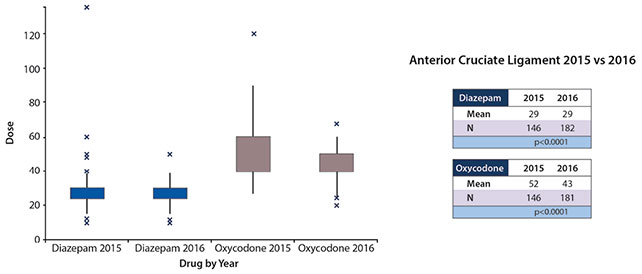
Prescriptions written for diazepam for patients who underwent spine surgery for AIS declined from 51 doses to 33 doses (P<0.0001; 95% CI -24.6 to -12.8) and oxycodone declined from 71 doses to 47 doses (p<0.0001; 95% CI -31.6 to -15.8) (Figure 3). Prescription written for oxycodone for patients who underwent surgical repair of a SCH fracture fell from an average of 34 doses per prescription to 22 doses (p<0.0001; 95% CI -14.9 to -8.1) (Figure 4). Prescriptions written for diazepam for patients who underwent a PAO decreased from an average of 45 doses per prescription to 34 doses (p=0.0113; 95% CI -20 to -2.6) and oxycodone prescriptions decreased from 59 doses per prescription to 47 doses (p=0.0190; 95% CI -22.7 to -2.1) (Figure 5). Prescriptions written for oxycodone for patients who underwent an ACL reconstruction dropped from 52 doses per prescription to 43 doses (p<0.0001; 95% CI -11.9 to -5.5), diazepam prescriptions remained constant between the years, 29 doses for both 2015 and 2016 (Figure 6).
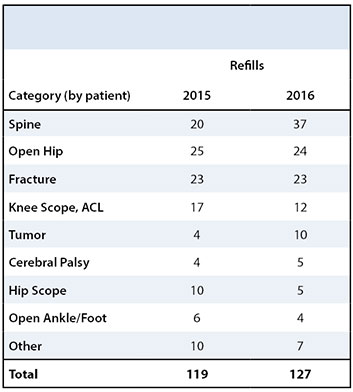
In addition to post-operative prescriptions, we also monitored changes in prescription refills between 2015 and 2016. In 2016, we found a slight increase in the number of diazepam (71 to 82) and oxycodone (99 to 117) refills. The total number of refills increased from 170 to 199. About half of the patients requested one refill per drug: 57% (97/170) in 2015 and 47% (94/199) in 2016. The remainder requested more than one refill. In 2015, seventeen patients requested refills twice, and five patients needed three or more refills. In 2016, twenty patients needed two refills, and thirteen needed three or more refills. As such, there were a total of 119 patients in 2015 and 127 patients in 2016 that requested refills.
There was some variation in the types of surgical procedures that patients requested refills after. The top four surgical categories after which patients requested refills remained the same: spine, open hip, fracture, and knee scope (including ACL) (Table 3). The most remarkable increase in refills between 2015 and 2016 was after spine surgery, where the number of refills increased from 20 to 37; tumor surgery also saw a big increase in need for refills, increasing from 4 to 10 patients.
The United States is experiencing an opioid addiction and overdose crisis, and this addiction often begins with narcotic prescriptions given by well-meaning physicians.12 As pediatric orthopaedic specialists, we are often prescribing opioids to help manage pain after surgery. The opioid prescriptions are, by the nature of the patient population, going into the homes of adolescents and young adults. While opioids are often necessary to help patients cope with acute post-operative pain, a few of these patients may convert to chronic pain. Ultimately, we wish to control the acute pain, without the conversion to chronic pain, while still not leading patients down a narcotic-dependent pathway.13 Furthermore, even in the absence of conversion to chronic pain, patients often have excess unused pills that remain in the house. These can then be discovered later and potentially used on a recreational basis.9 Motives for non-medical use of prescription pain medication may be different in adolescents, and the use of “leftover” pain medication for recreational parties is troubling.11,14 As many as 15% of 12th graders in the United States have taken prescription medicine on a recreational basis, typically stimulants and opioids.15 In a study of illicit drug use among adolescents, opioids accounted for 79% of the morbidity and 100% of the mortality in this population.8
The purpose of this quality improvement study was primarily to assess the current prescribing patterns of opioids in our department, to determine areas for improvement in the future. Additionally, because of recent legislative changes in Massachusetts, we could determine if our prescribing practices changed after the new legislation. When querying the residents, fellows, NPs and PAs, we found that these providers prescribe to the best of their ability, without truly knowing what an individual patient will need or use in the post-operative period. In general, the prescribing goals focus more on controlling pain than limiting excess narcotics. However, counseling about narcotic side effect and weaning is typically given. Most all providers note that their prescribing habits have changed since the new Massachusetts legislation.
We found a significant decrease in narcotic doses prescribed in 2016 when compared to the same timeframe in 2015 (before the Massachusetts legislation). This was true in general, as well as for specific procedures of ACL reconstruction, PAO, spinal fusion for AIS and surgical repair of SCH fractures. Interestingly, while the post-operative narcotic prescription doses decreased significantly from 2015 to 2016, this did not result in an increase in refill prescriptions for most diagnoses. However, in patients after spine and tumor surgery, we saw an almost doubling of the refill needs of this population. This indicates that while we successfully decreased our narcotic prescription dosing in response to the Massachusetts legislation, many of our post-operative spine and tumor patients may have been underserved by the one-week post-operative narcotic restriction.
In a separate study from our institution, patients after ACL surgery were contacted after the surgery for a “pill count” to determine the exact number of opioid pills prescribed and utilized in the post-operative period (Solodiuk J, personal communication). They found that while the narcotic prescriptions were for 40-60 pills, patients typically utilized 32% of what was prescribed. Clearly more work in this regard needs to be done.
Post-operative narcotic prescriptions are written without true knowledge of what patients need for certain procedures. As such, over prescribing is common. Yet with this current societal narcotic abuse problem, we, as prescribers, need to respond and change our prescribing practices.16 The surgeon general, the FDA, and even the Massachusetts legislature has taken notice of the opioid crisis.10,17,18 We also need to consider improving the education that training physician receive regarding opioid prescribing.19
Alternate pain treatment modalities are available and have been shown to be of benefit. Regional anesthesia, such as nerve blocks, may decrease pain, decrease narcotic use and potentially decrease cost.20 Routine use of non-narcotic medication, such as ketorolac and gabapentin may be effective, even in spine surgery.21,22 Further exploration of these alternate modalities to address post-operative pain while decreasing oral narcotic prescriptions should be done.
In the balance of trying to appropriately address post-operative pain while still not overprescribing opioids, we still need to make some improvements. Continued investigation into actual narcotic pill use for particular types of procedures is essential in order to streamline prescriptions for these patients. Additionally, ongoing exploration of non-oral pain modalities for treatment of post-operative pain needs to be pursued. And perhaps we need to consider legislation to improve the refill process for the few procedures (e.g. scoliosis surgery) where prolonged narcotic needs are anticipated.