Novel Intraoperative Technique for Thoracic Level Localization Utilizing a Percutaneous Upper Lumbar Intrapedicular Jamshidi Needle as a Fixed Marker for Wrong Level Surgery Avoidance: Technical Note and Literature Review
C. Chambliss Harrod, MD, Richard F. Rathbone, MD, Robert E. Boykin, MD, Kirkham B. Wood, MD
The authors report no conflict of interest related to this work.
©2015 by The Orthopaedic Journal at Harvard Medical School
OBJECTIVE To introduce a novel simple, cost-efficient, safe, reproducible intraoperative thoracic-level identification technique during open or minimally invasive posterior or lateral (transthoracic) approaches with the use of a Jamshidi needle anchored as a fixed marker in the upper lumbar spine.
BACKGROUND Wrong site or level surgery is an unfortunate problem in thoracic spine surgery that can compromise patient care. Likely under-reported, literature is sparse regarding risk factors and effectiveness of current protocols to prevent and decrease the frequency of wrong-level surgery. Accurate intraoperative thoracic spine level localization is often not easily achieved. Coordinating pathology on preoperative imaging with intraoperative imaging is even more difficult in patients with challenging anatomy and non-traumatic conditions. Typically, spot or live fluoroscopy with non-fixed markers (needles, instruments) is performed. Increased radiation exposure to both patient and surgeon results, and correct level identification is often difficult. Recent technological advances include radiographic placement of radiopaque embolization coils, screws, markers, or cement augmentation into the pedicle of interest. However, these techniques increase costs, require admission and increase length of stay, increase anesthetic and radiation exposure, and need additional confirmatory cross sectional imaging (CT or MRI) post-procedure.
METHODS Ten patients with nontraumatic etiologies including symptomatic thoracic disc herniations, ossification of posterior longitudinal ligament, epidural abscess, and osteomyelitis underwent surgical treatment via anterolateral, posterior, or combined approaches. Using standard percutaneous techniques, a standard Jamshidi needle was placed into the most cranial lumbar vertebrae (typically L1 or L2) that can be visualized on the same lateral fluoroscopic image as the sacrum using a true AP image to serve as a fixed marker to confidently and accurately reference more cranial levels throughout the case.
RESULTS Ten patients underwent successful thoracic decompressive and reconstructive procedures with correct level identification via the Jamshidi technique without complication.
CONCLUSION Combined with appropriate preoperative imaging, intraoperative placement of Jamshidi needles allows confident thoracic level identification of any (non-traumatic) pathology without the need for another procedure, anesthetic, cross-sectional imaging study or the additional radiation exposure, costs, or complications associated. It is a safe, efficient, and reliable thoracic level identification technique.
Wrong-level spinal surgery is an unfortunate source of frustrations for both surgeons and patients.1-3 Additional procedures, morbidity, cost, anxiety, and lack of trust frequently compromise patient care and the patient-doctor relationships, often culminating in litigation.2 Thoracic pathology requiring surgical intervention can be associated with a disproportionately high rate of wrong-level surgery in non-traumatic etiologies where a focal deformity or fracture does not readily identify correct levels. Accurate intraoperative thoracic spine level localization is often not easily achieved. Coordinating non-traumatic pathology on preoperative imaging with intraoperative imaging is even more difficult in patients with obesity or challenging anatomy. Traditionally, counting techniques using preoperative then intraoperative spot or live fluoroscopy with the use of extracorporeal radio-opaque markers such surgical instruments or needles are employed. These require increased radiation exposure to both surgeon as well as patients and can still be difficult to correctly localize levels. Other techniques include use of C7-T3 spinouts process anatomy, 2-D or 3-D fluoroscopic or computed tomography (CT)-based neuronavigation, preoperative radiographic placement of radiopaque embolization coils, cement augmentation, marking wires, or fiducial screw placements into the pedicle of interest.4-8 However, these techniques increase costs, often require admission (and increase length of stay), increase anesthetic and radiation exposure, and may necessitate additional confirmatory cross sectional imaging [CT or magnetic resonance imaging (MRI)]. To the best of our knowledge, we introduce a new cost-efficient, reproducible intra-operative thoracolumbar level identification technique. Ubiquitous to spinal surgeons due to use in both minimally invasive techniques as well as aspiration of bone marrow aspirate, we use the Jamshidi needle anchored as a fixed marker in the upper lumbar spine to definitively and confidently localize levels for thoracic spinal surgery regardless of minimally invasive or open posterior or lateral (transthoracic) approaches.
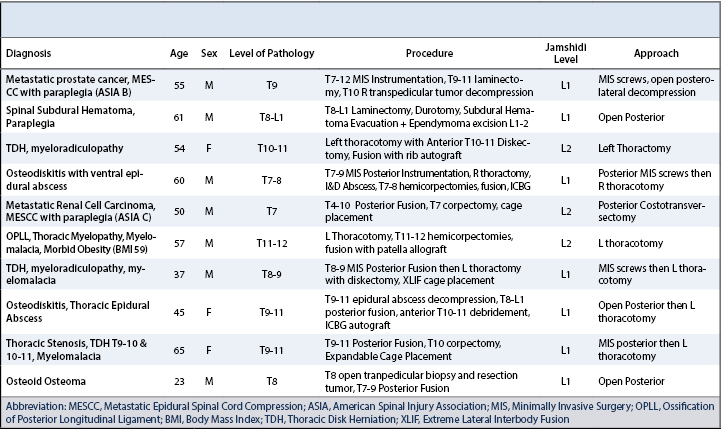
Ten patients with nontraumatic etiologies including symptomatic thoracic disc herniations, ossification of posterior longitudinal ligament, epidural abscess, and osteomyelitis underwent surgical treatment via a combination of minimally invasive and open lateral, posterior, and combined approaches (Table 1). Preoperatively, we employ routine thoracic [lateral, anteroposterior (AP)] and full length 3 foot standing scoliosis [lateral, posteroanterior (PA)] radiographs in addition to both thoracic and entire spine scout T2-weighted MRI sequences to denote the level of interest counting cranially from the sacrum with careful attention to possible transitional lumbosacral levels, number of non rib-bearing (lumbar) vertebrae and identification of the twelfth (or lowest) rib. Additionally when available, scout coronal thoracolumbar CT images (in addition or in place of plain radiographs) are quite helpful in identifying the twelfth rib and the number of lumbar vertebrae. We print and displayed all images in the operating theatre to confirm the number of lumbar vertebrae, presence of transitional anatomy, morphology of the twelfth rib, and ultimate labeling of thoracic pathology.
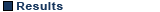
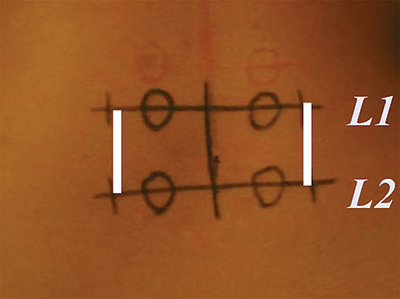
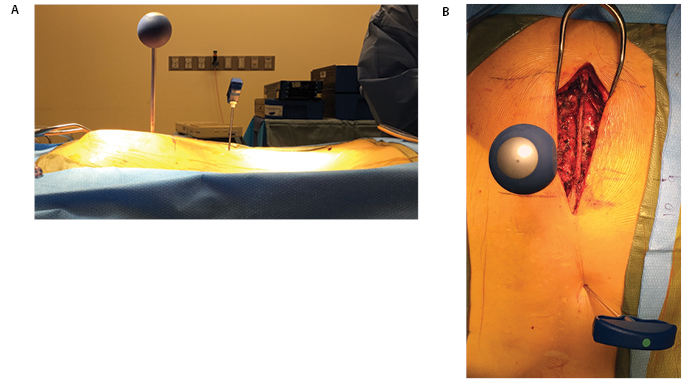
Patients are positioned on a radiolucent Jackson table either prone (with chest, hip, and thigh pads) or lateral with bolsters. The surgical field is prepped from the axilla (transthoracic approach) or cervicothoracic (posterior) junction all the way to the superior aspect of the gluteal crease below the posterior superior iliac spine. After draping, we then obtain a true AP fluoroscopic image of the uppermost (L1) lumbar (or first, non-rib bearing vertebrae) with the spinous process centered between the pedicles, whose superior border approximates adjacent superior endplate (Figure 1). Using a Kischner wire, we then mark the midpoint of the pedicle transversely followed by the lateral aspect vertically (Figure 2). If doing a transthoracic case, we utilize the ipsilateral (or “upside”) pedicle for technical ease. The Jamshidi needle is then inserted on the skin surface typically 2 cm lateral to the lateral wall of the pedicle and advanced until the transverse process is palpated (Figure 3). It is then “walked” medial until the junction of the transverse process and lateral upslope of the superior articular facet is tactilely felt with fluoroscopy confirming appropriate starting point. This technique avoids iatrogenic injury of a lumbar facet joint or capsule. Additionally, use of true AP imaging for marking the upper lumbar vertebrae can reliably identify correct levels even in the face of coronal or sagittal plane deformities so long as preoperative planning correlates number of non-rib bearing lumbar vertebrae with correlation to thoracic pathology.
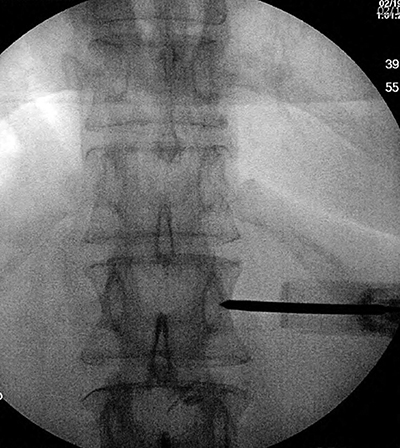
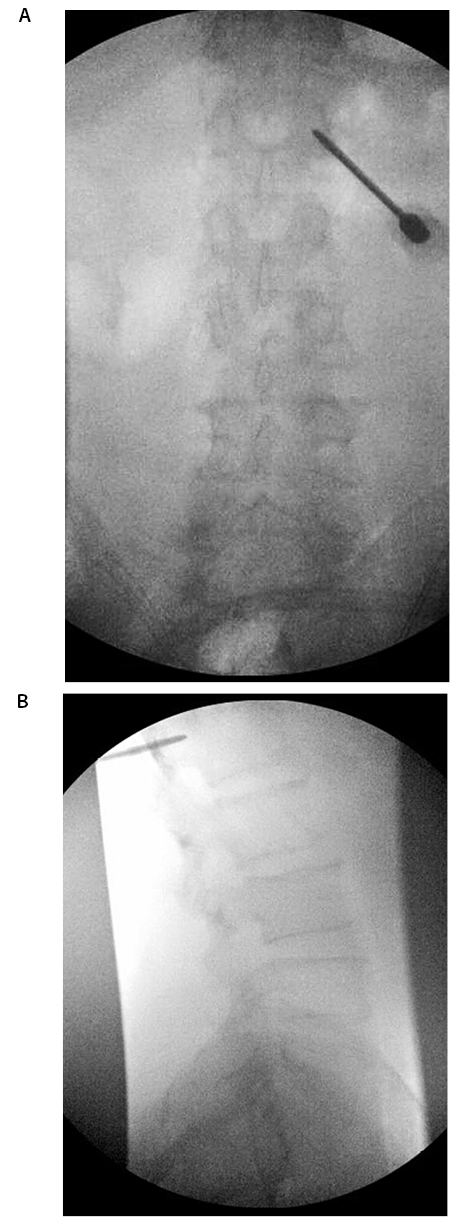
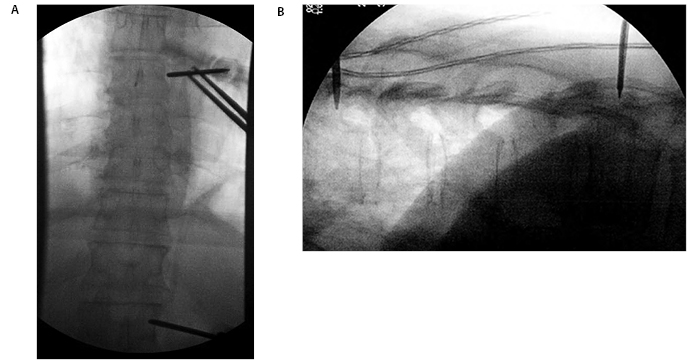
We then advance the Jamshidi needle via mallet impaction typically 15-20 mm but always stopping prior to reaching the medial border of the pedicle (Figure 4A). A lateral fluoroscopic image is then obtained with the Jamshidi and the lumbosacral junction visualized in a single image to confirm the appropriate marking level (Figure 4B). Similarly, the fluoroscope is moved cranially and typically T8 (+/- one level) can be visualized and definitively counted from the Jamshidi marking level (typically L1, occasionally L2) (Figure 5). If the desired level is more cranial, the steps are repeated for placement of a thoracic Jamshidi in similar fashion as above with the only caveat being slightly more care taken to avoid incidental medial displacement of the needle towards the canal due to the orientation of thoracic transverse processes when obtaining an initial starting point. The definitive level(s) are then marked for a lateral or posterior case with subsequent operation performed. We leave the Jamshidi needle in the upper lumbar vertebrae until the end of the case serving as a continual fixed reference point once deep exposure of the levels has been performed for a repeat counting for final level confirmation prior to undertaking any definitive decompressive or reconstructive procedure (Figure 6). It also allows final images to be obtained when constructs are utilized in reconstructive procedures.
All ten patients underwent correct thoracic level identification, exposures and subsequent decompressive and/or reconstructive procedures using the above technique without complication. In addition to expected and appropriate clinical response, postoperative imaging included full-length postoperative scoliosis radiographs to visualize entire thoracolumbar spine prior to discharge to ensure accurate levels compared with preoperative imaging. Routine use of postoperative CT or MRI was not employed.
The Joint Commission (JC) broadly defines “wrong site surgery” as any surgery performed on the wrong site or patient or performance of the wrong procedure.9 Wrong level “exposure” involves surgical exposure on an unintended level but not implying incorrect surgery performed. In a prospective study of 100 lumbar discectomies, Ammerman et al. report a 15% rate of inappropriate exposure.10 Wrong level “surgery” involves performing surgical procedures (essentially, decompression or fusion/instrumentation) at the wrong level or part.11 Wrong level surgery commonly results in complex medical, legal, social, and emotional issues for both the patient and physician involved.12 Although seemingly rare (0.09 to 4.5 per 10,000 surgeries performed), about half of spine surgeons will experience a wrong-level surgery during their career.2, 13, 14 The American Association of Orthopaedic Surgeons (AAOS) in 1997 advocated patients place initials on the operative site.15 The North American Spine Society (NASS) advocated the “Sign, Mark, and Radiograph” protocol in 2001 with a similar JC protocol issued in 2003 in an effort to reduce incidence of wrong-level operations.16, 17 However, Wong et al. reported a rise in wrong site surgery events after instituting the JC Universal Protocol although it was not known if there was a true increase in wrong site surgery versus increased awareness and reporting.18 A paucity of high-quality literature exists; however, a multitude of risk factors have been proposed. Most notably, failure to use fixed site markings, inappropriate positioning, inadequate preparation/preoperative planning, emergent operations, and anatomical anomalies are often cited.
In addition to following the above protocols, Devine et al. in a systematic review of the wrong-level surgery most strongly recommended intraoperative imaging after exposure and marking of a fixed anatomic structure that can be directly compared with preoperative studies to determine the correct site for spine surgery.2 In particular, thoracic procedures are disproportionately at risk for wrong-level operation as multiple anatomical challenges including distance away from known reference points (lumbosacral junction or C2), ribs complicating counting techniques, lumbar vertebrae variability (number, presence of transition anatomy), and difficulty imaging due to obesity. A key step in preventing wrong-level surgery is meticulous scrutiny of preoperative imaging with the surgeon understanding and documenting his own method of level derivation that can be reproduced with certainty in the operating theatre with the use of radiographs or fluoroscopy. Each surgeon must have his own method of definitively determining the pathological level. As described above, we always begin with plain radiographs (thoracic, scoliosis) in addition to cross sectional imaging (thoracic and entire spine scout MRI with or without CT) as we will be directly correlating intraoperative fluoroscopic radiographs to our preoperative radiographs during surgery. When CT is indicated (OPLL, understanding disk calcification, fractures), it is immensely helpful in identifying the twelfth rib and the number of lumbar vertebrae. Correlating the official radiologist interpretation and accepting or rejecting (with documentation reasoning) eliminates surgeon confusion on the date of surgery as well as provides solid reasoning if one labels the level of pathology different from the radiologist. Once more, we recommend physically printing and displaying these images in the operating theatre for continual referencing in the OR and as a backup if portable disks or internet-based imaging is unable to be retrieved.
Other level identification methods have evolved over time as technology has improved. Prior to the advent of fluoroscopy, posterior counting techniques required more extensile exposures so that the first non-rib bearing (C7 or L1) vertebrae can be identified (nearly always caudally referenced from L1) or counted from C7-T3 spinous process anatomy.4 Currently, intraoperative imaging is the standard of care with radiation exposure to both patient and surgeon previously quantified depending on both location (lumbar > cervical) and modality (CT > fluoroscopy or radiographs).19, 20 Most commonly, counting techniques utilize fluoroscopy with the use of extracorporeal radio-opaque markers such surgical instruments or needles are employed. These require increased radiation exposure to both surgeon as well as patients and can still be difficult to correctly localize levels. Other techniques include use of 2-D or 3-D fluoroscopic or CT-based neuronavigation, preoperative radiographic placement of radiopaque embolization coils, cement augmentation, marking wires, or fiducial screw placements into the pedicle of interest.4-8 However, these techniques increase costs, often require admission (longer length of stay), increase anesthetic and radiation exposure, and may necessitate additional confirmatory cross sectional imaging (CT or MRI). A need remains for a cost-efficient, safe, simple, reproducible intraoperative thoracic level identification technique by which any thoracolumbar level may be easily identified regardless of pathology or deformity. Avoidance of additional radiological or interventional procedures with possible complications and increased radiation exposure (to both patient and operator) is possible with our technique using a percutaneous upper lumbar Jamshidi needle placement to serve as a fixed marking anchor by which all cranial levels can be confidently labeled.
Although we did not experience any complications, strict adherence to the above technique is recommended to avoid inadvertent facet violation and potential slippage of Jamshidi needle with injury to adjacent structures. Lastly, premature removal of the Jamshidi marker at any point during the operation could increase risk for wrong-level operation.
Combined with appropriate preoperative imaging, intraoperative placement of Jamshidi needles allows confident thoracic level identification of any (non-traumatic) pathology without the need for another procedure, anesthetic, cross-sectional imaging study or the additional radiation exposure, costs, or complications associated. It is a safe, efficient, and reliable method of localizing thoracic spine levels intraoperatively that utilizes technique familiar to all spinal surgeons.